As a private physician, I work each day to improve the lives of my patients. Not through pointless 15-minute visits and thoughtless prescriptions, but by providing comprehensive and personalized attention to every patient, every time.
I’m proud of what Brentwood MD has accomplished, but I couldn’t have done any of it without my right-hand woman. Jen Justus is equal parts genius and nurturing.
She’s been a registered nurse for 23 years and recently achieved the title of Nurse Practitioner. Her clinical experience unexpectedly opened Jen’s eyes to the complex and intricate nature of women’s health issues. And, she is the perfect guest for me to discuss the topic of women’s health.
“The needs of women throughout their lifespan change so much. They come into the doctor with hot flashes, depression, and so many other symptoms triggered by hormone changes,” Jen says. “But their doctors just start them on medications like antidepressants that don’t work long term.”
Jen has joined me to discuss the important implications of hormone replacement therapy for women. There’s only one place to begin this discussion: back in the 1980s when women’s health finally earned its place on the map and became a political priority.
An Introduction to the Women’s Health Initiative
The Women’s Health Initiative changed the game for women’s health, for better and for worse. While it drew attention to many of the significant issues faced by aging women —menopause, stroke, heart disease, hip fractures, and breast cancer — it also inadvertently made an already confusing topic even harder to understand.
Overall, the Women’s Health Initiative was a long-term national health study that focused on preventing heart disease, cancer, and osteoporosis in postmenopausal women. It became one of the largest women’s health projects ever launched in America, with 161,808 women enrolled at 40 clinical centers around the country.
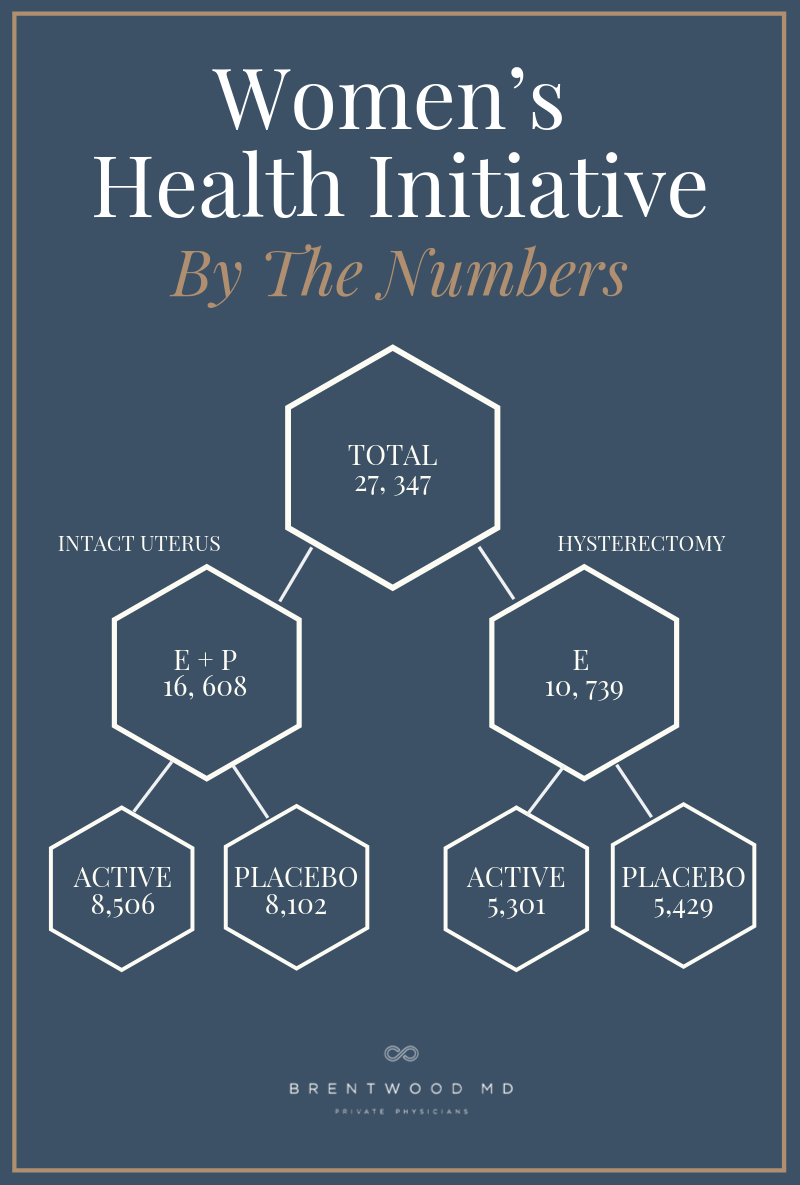
Those 161,808 women were split between a clinical trial, an observational study, and a community prevention study. The clinical hormone trials studied 27,347 postmenopausal women ages 50 to 79 years between 1994 and 2004.
According to the National Institute of Health (NIH), the WHI Hormone Therapy Trials were designed “to test the effects of postmenopausal hormone therapy on women’s risk for coronary heart disease and on hip and other fractures and breast cancer.”
Why Did the Government Fund the WHI?
Though we’d like to believe that research studies occur as a result of human curiosity and generosity, the truth is that all research efforts are driven by some political or economic force. This is especially true for trials run by the government and pharmaceutical companies.
I can’t help but wonder: why did the federal government feel the urgent need to suddenly divert so much attention to women’s health in the early 1990s? It allocated $300 million and 20 years of manpower to the WHI, while negatively impacting other government-funded grant projects in the process. The answer, of course, has political undertones.
Back in the mid-1980s, women were rarely, if ever, elected to political positions in our country. The Good Ol’ Boys Club was still going strong, and only 13.5% of all grant dollars were dedicated to improving women’s health. The government’s spending habits emphasized the uneven attention given to male and female hormones. Of the money generated from that 13%, funds were disproportionately spent on fertility and pregnancy issues, with not a single study or insight into the long-term health and morbidity of women beyond childbearing age.
As patterns emerged showing chronic disease claiming more and more female lives, pivotal public and political figures finally started to ask why? It was around this same time that women gained traction in political forums and gave a stronger voice to females across the country.
The Women’s Health Initiative was the government’s answer to those calls for an equal representation between men’s health research and women’s health research.
How Were the WHI Hormone Therapy Trials Organized?
The WHI Hormone Therapy Trials were split into two main sections based on whether the participants had undergone a hysterectomy to remove their uterus. Women with an intact uterus created one group, and women without a uterus created the other section.
Due to the well-documented connection between unopposed estrogen and uterine cancer, only women who had undergone a hysterectomy received synthetic estrogen therapy alone (E-Alone). All other women received a synthetic estrogen and progestin blend (E + P). Each group also had a placebo group, which created a total of four study sections.
It’s essential to understand how this study was organized to appreciate its results. Even today, more than 20 years later, the top Google headlines for this study include titles like “WHI Study Data Confirm Short-Term Heart Disease Risks of Combination Hormone Therapy for Postmenopausal Women” and “WHI Follow Up Study Confirms Healthy Risks of Long-Term Combination Hormone Therapy Outweigh Benefits for Postmenopausal Women.”
Those are very strong statements to make, especially given the nuances of the data and the weaknesses of the study. As practitioners who believe in the power of bioidentical hormones, I believe that Jen and I have a moral obligation to help women understand this confusion and weigh the benefits and dangers of hormone therapy objectively.
The WHI Hormone Therapy Trial Results
During the WHI Hormone Therapy Trial, The E-Alone and E+P groups were given a single daily oral dose of synthetic hormones, either estrogen or estrogen with progestin. Keep this in mind, since there’s a huge difference between the synthetic hormones used in this study and the bioidentical hormones available today.
After nearly a decade of research, the hormone therapy trials ended early after the WHI Data and Safety Monitoring Board evaluated the data. They made the determination that the risks of the program outweighed the benefits. But what was the data, exactly?
The narrative of the WHI is set in stone — Hormones are so dangerous! Stay away from replacement therapy! — but the raw data combined with the limitations of this study contradict the narrative.
Understanding Why the WHI Hormone Therapy Trial Ended Early
Overall, the data demonstrated an increased risk of stroke among the E-Alone group. For every 10,000 women in the E-Alone group, 12 additional strokes occurred compared to the control group. Now, nobody can argue that one stroke is one too many, but does the addition of 12 strokes across 10,000 older women constitute the claim that all hormone replacement therapy is too dangerous to continue?
It’s also important to consider that the women in the E-Alone group were generally older and obese with high blood pressure. Their pre-existing conditions set the stage for negative outcomes since they were predisposed with specific risk factors. Yet the reports of the study, even to this day, don’t consider these conflicts and limitations.
Conveniently, this narrative also leaves out the fact that the E-Alone group did not experience an increase of invasive breast cancer, colon cancer, or hip fractures. The stroke data muddied the waters and created broad, extrapolated conclusions that blurred the facts.
We also can’t overlook the fact that medicine is an entirely different process today. The conclusions being drawn from this data are now more than two decades old. If this study was performed again today, the processes, procedures, and data collection techniques would be completely different. Are we blaming male and female hormones when that’s not the full story?
What Was Significant About the Estrogen Used in the Trial?
More than anything else, it’s critical to understand that the estrogen and progestin used in the WHI Hormone Therapy Trials were synthetic hormones.
Synthetic estrogen is derived from the urine of pregnant horses and made in a lab. This means that the estrogen used in the WHI trial was nowhere near what the female body produces naturally.
Jen explains the core difference between synthetic hormones and bioidentical hormones. “Bioidentical hormones are completely different, they are compounded in a pharmacy and made true to the molecules that our ovaries create.”
In other words, bioidentical hormones aren’t meant to merely mimic or look like estrogen. They are the same molecules as natural estrogen.
Jen says, “Estrogen is always seen as the bad guy.”
When in reality progestin is the synthetic hormone that robbed the bank and escaped. Research now shows that synthetic progestin is associated with higher risks of breast cancer and other complications when compared to natural progesterone.
How to Choose the Right Hormone Therapy
With misinformation and poorly drawn conclusions more prevalent than the objective truth, how can you decide whether hormone replacement therapy is the right choice for you?
Jen shares a powerful story that demonstrates the importance of understanding your choices.
“My mom recently shared with me that when she went through menopause she took a synthetic combination of estrogen + progestin, and she ended up with breast cancer,” says Jen. “Can you make the correlation between the two? Yes, but I don’t know if they caused the cancer. Having that in my family history makes the bioidentical hormone conversation even more important for me. I want to age gracefully, I want to live a long time, I want to have strong bones, I don’t want these chronic diseases.”
Jen and I believe in the powerful potential for bioidentical hormone therapy to improve female health, but we also don’t believe in one-size-fits-all solutions. We can’t stand on a soapbox and declare “All women need to supplement with bioidentical estrogen!” any more than the WHI can claim that hormone therapy is dangerous for all women.
The question is, does it provide more of a benefit than a risk to supplement your hormones to an optimal level once they start under-producing?
We don’t have the large-scale bioidentical hormone studies to prove it since the government and pharmaceutical industries can’t make money from bioidentical hormones.
Nevertheless, we believe the proof is in the success stories we witness every day. Even when you sift through 50 years worth of U.S and European studies, you won’t find a single study claiming that bioidentical hormone therapy causes harm.
We have to make decisions for ourselves and our loved ones, so Jen’s advice is the best out there: “Find a provider that can explain, intelligently and objectively, how hormone therapy may impact your health.” Then decide how you can take that information and apply it to make the best decisions for your own life.
You deserve to feel amazing, reduce excess fat, prevent disease, and remain active and vibrant into your 7th, 8th, 9th, and 10th decade of life. Jen and I believe bioidentical hormone therapy can most likely help you achieve that goal.
In the End, What Did the WHI Study Really Prove?
The Women’s Health Initiative hormone study claimed to “prove” a lot, but it’s our job to sift through the noise and find the truth. Synthetic hormones aren’t safe, but the simple presence of supplemental estrogen helped some women achieve positive health results in the trial period.
If we can take the concept of hormone replacement implemented in the WHI trial, but use bioidentical hormones instead, the options are endless.
“What a wonderful time to be a woman in the healthcare spectrum right now,” Jen says. “Our screening tools for cancer are top-notch, our education and training about longevity are better than ever. Up until the WHI study, women were treated the same as men in the medical community. It took this study to say, hey, women are dying, and we need to find out why.”
Jen’s right. Regardless of the conflicting data produced by the WHI study, one thing is undeniable. Women’s health finally came to the forefront as a topic that needs (and deserves!) to be fully explored, and now women receive infinitely better care as a result.

Dr. Aaron Wenzel is a concierge physician specializing in the care of fast-moving entrepreneurs, executives, and public figures in the Nashville, TN area. Dr. Wenzel’s diverse life experience and extensive training in family medicine, emergency care, nutrition, and hormone replacement therapies give him the unique platform to provide unmatched care for his patients.







