Hormone optimization is one of the most important and misunderstood health therapies available today. My partner in crime, Jen Justus, and I have been eager to dive into the details of this conversation specifically for women; we’ve been holding up the dam, waiting to share this valuable hormone optimization content until the time was right.
Jen is extremely passionate about this topic. As a Nurse Practitioner and registered nurse for more than 23 years, Jen has witnessed firsthand the consequences of hormone deficiencies, as well as the incredible benefits of bioidentical hormone therapy.
Let’s dive right into the conversation that women need to have in order to understand the truth about bioidentical hormone therapy and optimization. Could it be the answer you’ve been waiting for?
What is a Hormone?
Hormones are produced in glands throughout the body as part of the endocrine system. We all have a general understanding that hormones influence our most important body functions, but the details are fuzzy.
Most of the confusion surrounding hormones develops because we discuss hormones like they exist in a vacuum. However, the endocrine system is anything but a vacuum. It’s a complex give-and-take system, where one action or change affects ten others. Most hormone changes occur simultaneously, not in a vertical, organized process like we imagine.
As Jen describes, hormones are chemical messengers. “They’re little molecules that are busy in our bodies. Sometimes they peak at different times in the month, and they all interplay with each other,” she says.
“Unfortunately, as we age, they don’t become less important, but they become less abundant. That’s where a lot of us feel the effects of not having enough hormones in our bodies.”
With so much confusion around the topic of hormones, even people who are genuinely interested and curious about hormone optimization may struggle to find a safe and objective place to pursue a conversation about hormones. You deserve to understand what hormones mean for you currently and as you move forward in your postmenopausal health journey.
Normal Vs. Optimal Hormones
One of my core beliefs, as Jen can tell you, is that the goal in life is not to survive. Ants survive. Mice survive. But humans should thrive. We are capable of experiencing life at an optimal level, not just a survival level.
But this wasn’t always the case! We’ve entered uncharted territory in the 21st century because our overall life expectancy has never been higher. Ancient Greeks and Romans rarely made it out of their twenties, and life expectancy hovered between 30 and 40 years of age from the 1500s until the 1800s. Even in the 1940s, the average life expectancy was barely above 60.
Today, however, life expectancy has surged past 80, and living to 90 is becoming increasingly commonplace. So 90 is really the new 60! We’re facing the reality that most of us will continue living on this planet for decades longer than our grandparents and great-grandparents did. This changes how we approach everything, from our financials and our relationships to our healthcare.
Our entire belief system needs to shift and force us to change what we consider to be normal. If you hang up your hat at age 55, you might still have a full 30 or 40 years to fill! How are you going to spend that time? Will you survive, or will you thrive?
Personally, I’m not interested in a normal life. I want an optimal life where I’m the best person, physician, husband, and father that I can be. It turns out that bioidentical hormones can be the key to help you live up to the best version of yourself.
What Hormones Do Women Need to Be Mindful Of?
Bioidentical hormones are identical to what your body produces, which is the reason why we’re such advocates for them. However, not all hormones are created equally — not even close.
Synthetic hormones are processed in a lab. They’re not identical to the hormone molecules our bodies make.
They’re a close look alike, but they’re not the real thing.
Intuitively, you know it’s better to replace whatever you’re missing with a natural alternative. But there’s no economic or political benefits for pharmaceutical companies or government agencies to fund large scale bioidentical hormone therapy research studies. As a result, we don’t have the hard data to prove what we know intuitively and anecdotally.
Pharmaceutical companies will devote time, energy, and resources to research studies when they see the opportunity to patent (and therefore monetize) a specific chemical or formula as a result. Bioidentical hormones can’t be patented, since they are identical to human hormones. No patent, no money, no research.
But Jen and I don’t need a $300 million research study to confirm what we already know —bioidentical hormones have the ability to safely and effectively optimize your health and your life.
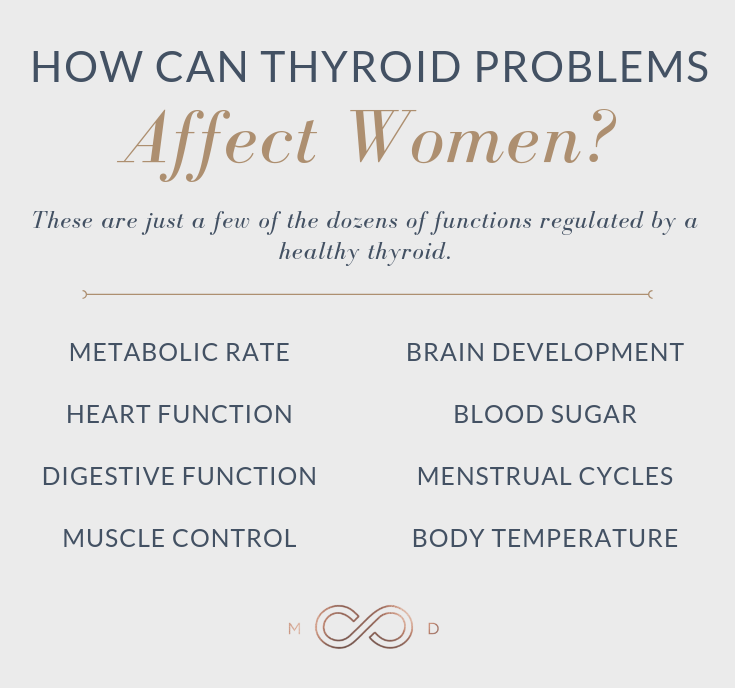
How Can Thyroid Problems Affect Women?
Thyroid problems, especially primary hyperthyroidism, affect women at a disproportionate rate compared to men. In fact, women are 5 to 8 times more likely to experience a thyroid imbalance than their male peers.
Even though the thyroid is a small gland at the base of your neck, it plays a critical role in your overall wellness. The thyroid works with your bloodstream and brain to produce and release thyroid hormones used to perform essential metabolic functions.
The following list shows just a few of the dozens of functions regulated by a healthy thyroid:
- Metabolic rate
- Heart function
- Digestive function
- Muscle control
- Brain development
- Mood
- Menstrual cycles
- Body temperature
- Blood sugar
- Cholesterol
A healthy thyroid maintains just the right levels of its hormones, which helps your body to achieve optimal functionality and health. When the thyroid struggles to produce its hormone, the differences of optimal vs suboptimal become clear. Chronic symptoms quickly develop, including missed menstruation, weight gain, fatigue, irritability, always feeling cold, and intense fatigue are a few of the most common.
Thyroid disorders like primary hyperthyroidism are still some of the most untreated and mismanaged diseases, despite the advanced tests and tools we have to treat it efficiently.
Some doctors don’t want to engage in comprehensive thyroid conversations (and how could they in a rushed six-minute appointment?). Other doctors assume that a pill can solve thyroid problems, and they never peek out of the box to consider holistic solutions or re-evaluate misleading lab tests.
You need to find a physician who won’t mismanage your thyroid diagnosis, someone who can properly identify your condition and treat the symptoms you’re experiencing.
Should You Consider Estrogen Replacement Therapy?
Poor estrogen. It has taken the fall for so much of the hormone discussion, even though it’s largely innocent.
Overall, estrogen is a sex hormone produced in the ovaries that helps a young girl develop into a woman. It influences menstruation, feminization of the body, ovulation, and fertilization.
If you look at most girls and women in their prime of estrogen production, say between the ages of 12 and 40, they’re vibrant, strong, energetic, and stable. They have regular periods, no signs of heart disease, and generally steady health. Women under the age of 55 rarely have heart attacks, a fact that’s directly correlated to the impressive cardioprotective effects of estrogen.
However, the rate of women with heart disease spikes after age 55. Heart attack rates for postmenopausal women outpace the rates of their male counterparts! It’s no coincidence; without the cardioprotective effects of sufficient estrogen production, women have to navigate a minefield of chronic disease.
Unlike the gradual decrease that men experience as they lose testosterone, women can lose their estrogen overnight.
Jen puts it best: “Our estrogen doesn’t just decrease slowly over time like a man’s testosterone. When menopause hits, the ovaries stop producing estrogen immediately. So we see brain fog, moodiness, weight gain, anxiety, depression.”
Vaginal dryness, atrophy, UTIs, urinary incontinence, and pain during sex are also huge factors in estrogen loss, but so many women are too embarrassed or ashamed to admit these symptoms. It’s difficult to divulge such personal details to a stranger, and they’d rather suffer in silence. But thanks to bioidentical estrogen therapy, it doesn’t have to be that way!
So who is bioidentical estrogen therapy for? “We won’t really start having the conversation until you’re fully in menopause — 12 consecutive months without a menstrual cycle. We also check to make sure hormone pathways are no longer responsive,” Jen explains.
At Brentwood MD, we use oral Estradiol, a bioidentical hormone, for postmenopausal women. We choose to use the oral form because it offers the best cardioprotection for women at risk of heart disease, stroke, and heart attack. The exact dose depends on each patient’s health, but we aim for a range between 75 and 100.
The benefits of bioidentical estrogen therapy speak for themselves:
- Reduction of cardiovascular disease
- Less breast cancer
- Bone health
- Protection from osteoporosis
It becomes easy to differentiate optimal vs suboptimal hormone levels after you experience the equalization achieved through hormone therapy.
How Do Estrogen and Progesterone Work Together?
Progesterone, estrogen’s dancing partner in the body’s careful hormone waltz, is a powerful addition to estrogen therapy because it prevents breast and uterine cancer. Simply put, you can’t take estrogen without also taking progesterone.
However, unlike estrogen, some patients can benefit from progesterone therapy before menopause. Its mood stabilizing and calming effects are known to alleviate intense PMS issues and help perimenopausal women sleep.
“The women in our practice who use progesterone therapy come in feeling more balanced,” Jen says.
A range between 10 to 30 ng/mL is a safe goal for progesterone therapy, and 20 ng/mL is ideal for most women.
Does Testosterone Really Matter For Women? Yes!
Testosterone is widely known as the male sex hormone, but its nuances might surprise you.
Aside from its critical role in male development and sexual health, testosterone is probably the most underrated hormone for women. Females do produce a small amount of testosterone in the ovaries. Young, vibrant women have optimal testosterone levels, but they decline as ovary function misfires.
Even though testosterone isn’t a huge driver in the female experience, its deficiency manifests itself in ways that can threaten a woman’s health and quality of life. Women suffering from testosterone deficiency often experience:
- Loss of libido
- Lower Drive
- Increased body fat %
- Lower Energy
- Lower Muscle tone
Bioidentical testosterone replacement therapy for women can be an invaluable tool to put the light back in your eyes. We see patients all too frequently who seem to have a version of themselves that they’ve lost. They want that version to come back out and help them be productive and driven, but it’s too difficult. Once we balance their testosterone levels, these women come back into themselves. The fire in their belly starts burning again.
Jen talks to women every day who feel unsure about testosterone therapy. “I would typically think of testosterone as the male hormone. Bodybuilders come to mind,” she jokes. “When we meet with our female patients, these issues come up. ‘Will I grow a beard!? I don’t want to get too buff!’ But we use tiny amounts, just fractions, to bring levels back into balance.”
Though any level between 0 and 10 is considered “normal”, we find that levels between 6 and 8 produce the best results.
Who Are Hormones Not For?
Jen and I have witnessed the transformative power of bioidentical hormones time after time, but we know that this therapy isn’t for everybody. Patients with any active cancer or a history of hormone-sensitive breast cancer shouldn’t undergo hormone replacement therapy at all. Patients with a non hormone-sensitive breast cancer and who are now cancer free, along with any significant family history of breast cancer should check with their doctor about risks vs benefits. We’re always willing to explore the option with patients who beat cancer or have a unique family history, but we tread lightly and dig deep into health profiles to ensure the safety of every patient.
Women considering pregnancy should also be careful to avoid estrogen and testosterone therapy. Testosterone in particular is very dangerous to a growing fetus, so there should never, ever, be an overlap between conception and testosterone therapy.
Considering Hormone Optimization For Your Health
Women hit menopause by 60 but are likely to live until 90. This gives you three or four decades of life to enjoy as a postmenopausal woman. How will you protect and enhance your health during that time?
It’s not the answer for everyone, but bioidentical hormone optimization may play a huge role in giving you the best life possible.

Dr. Aaron Wenzel is a concierge physician specializing in the care of fast-moving entrepreneurs, executives, and public figures in the Nashville, TN area. Dr. Wenzel’s diverse life experience and extensive training in family medicine, emergency care, nutrition, and hormone replacement therapies give him the unique platform to provide unmatched care for his patients.