Download file | Play in new window | |
I recently had the privilege of sitting down with Brooke Faught, a Doctor of Nursing Practice who has dedicated her career to women’s sexual and pelvic health.
In our previous discussion, we explored women’s sexual wellness and the complexities of low libido. This time, I wanted to dive deeper into another of Brooke’s areas of expertise: safe hormone management for women navigating perimenopause and menopause.
Brooke brings over two decades of experience to these conversations. As the founder of the Women’s Institute for Sexual Health and current Director of Women’s Health at Pazona MD, she’s witnessed firsthand how the medical community’s approach to hormones has evolved — for better and worse. Her expertise as a certified menopause practitioner through the Menopause Society and her fellowship with the International Society for the Study of Women’s Sexual Health give her a unique perspective on critical issues.
Beyond her credentials, Brooke’s passionate advocacy for women’s health has led to significant impact in the field through her research, publications, lectures, and even lobbying efforts.
The Reality of Hormone Testing: When Blood Work Helps and When It Doesn’t
One myth Brooke addressed is the assumption that hormone problems require extensive testing. New patients frequently ask her to check their hormones, hoping to find the reason for their symptoms. Brooke understands. “They just want to check something. They don’t feel their best.”
In reality, Brooke says, hormone testing isn’t always necessary. “In many cases, we can go based on symptoms.”
Take menopause, for example. “If a woman stops menstruating for a year, she’s officially menopausal. I don’t need blood work to confirm that,” Brooke notes.
However, Brooke finds hormone testing valuable in certain specific situations. When using off-label treatments like testosterone for women — since there’s still no FDA-approved testosterone specifically for women in the United States — testing helps her ensure hormone levels remain in a safe range. Additionally, if a patient doesn’t respond to treatment as expected, hormone testing and other blood work can provide insights into what else might be happening beneath the surface.
The key is individualization. Brooke considers factors like age, menstrual cycle status, and the presence or absence of a uterus when determining whether testing is necessary. Even details about when a patient’s mom, grandma, or aunts went through menopause provide valuable context, since patterns often run in families.
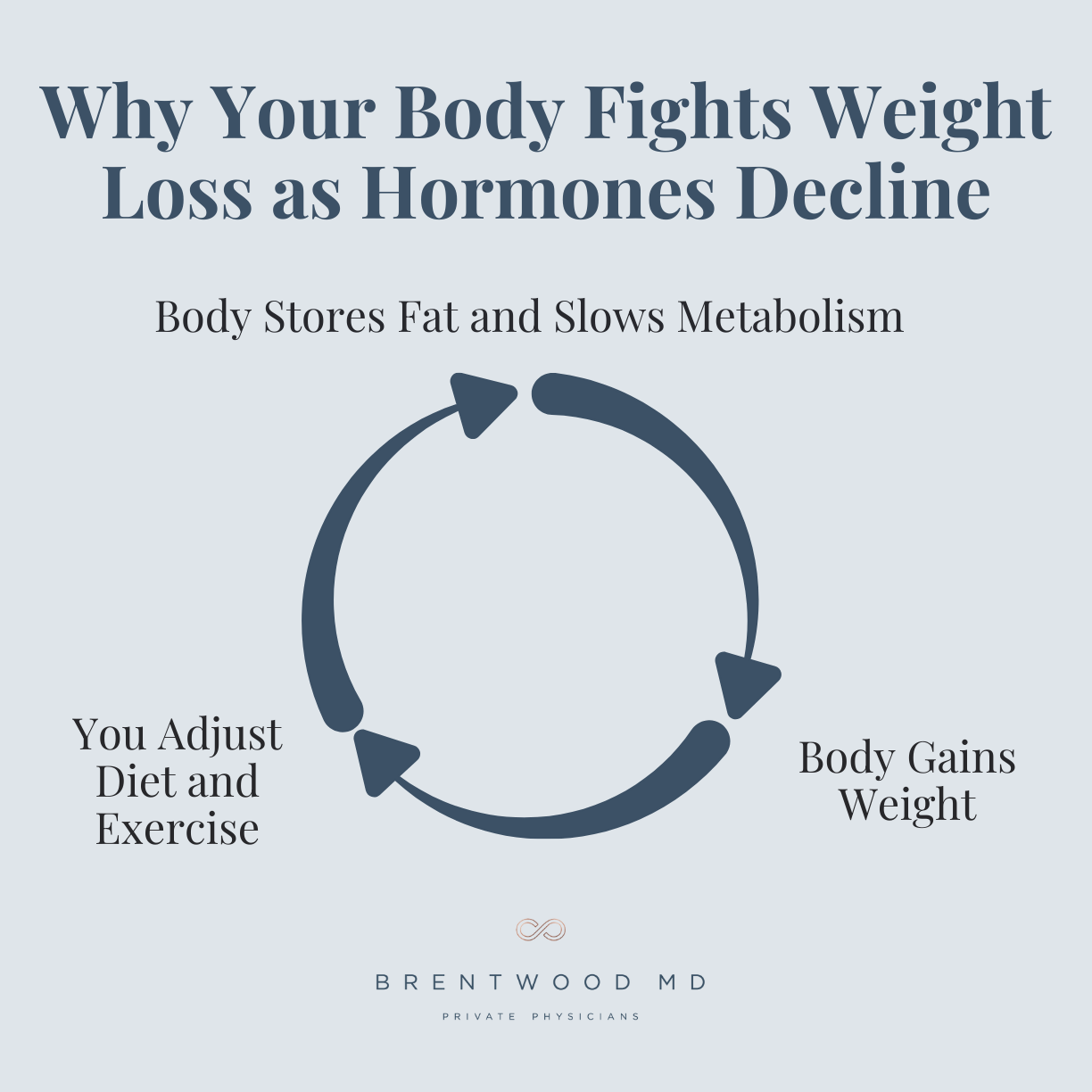
The Perimenopause Challenge: Why Your Body Fights Weight Loss
Perhaps one of the most frustrating aspects of perimenopause for many women is the seemingly overnight change in their ability to manage weight. You’re eating the same foods and maintaining the same exercise routines as before, yet the scale continues to climb.
Brooke’s explanation for this phenomenon was genuinely mind-blowing to me. “Our bodies recognize that there’s a change happening,” she explains. “Our bodies are smart, and they’re like, ‘I got you. I’m going to protect you. I’m going to hold on to resources.’”
In this case, your body “helpfully” slows your metabolism up to about 30% so you don’t burn through calories as quickly. Additionally, as it notices a reduction in hormone production, your body begins to store more fat cells, particularly around the midsection. Why? Because fat cells store hormones, and your body is hoarding.
If only you could tell your well-intentioned biology, “No, thank you. I’d really rather you didn’t.” Instead, your body chugs along, working directly against your weight management efforts as a survival mechanism. You may increase activity and decrease calorie intake, but it’s difficult to make a full 30% shift. Even if you do, your metabolism will likely shift even further to compensate.
These concerns aren’t about vanity. They’re about your health and quality of life — and discovering what’s happening in your body so you can respond appropriately.
Many women feel like they’re losing their minds when these and other changes occur seemingly overnight, but Brooke’s clear, biology-based explanation provides both validation and clarity.
Debunking Hormone Dangers: The Real Story Behind the Fear
When I asked Brooke about hormone safety — a topic shrouded in fear for over two decades — she provided crucial historical context I wish I had learned in medical school.
The fears surrounding hormone replacement therapy stem largely from the Women’s Health Initiative study, released in 2002. Brooke calls it “the gynecologic 9/11” because of how dramatically it changed the medical landscape. “We went from believing that everybody should be on hormones to nobody should be on hormones,” she recalls.
Here’s what most people — including many healthcare providers — don’t know about the study: It examined a very specific population using very specific hormone formulations. The researchers weren’t studying typical perimenopausal women experiencing common symptoms. Instead, they studied older, higher-risk women and gave them high-potency oral synthetic hormones.
When complications arose in this high-risk population, the medical community extrapolated those findings to all hormone use for all women. “Lengthy backstory,” Brooke acknowledges, “but I try to explain that to my patients so they understand where all this fear comes from.”
The current understanding of hormone safety focuses heavily on timing. Within the first 10 years of menopause, blood vessels remain relatively elastic and can accommodate hormone-rich blood effectively. After about 10 years without circulating estrogen, blood vessels lose some of their elasticity, increasing the risk of introducing hormone therapy at that stage.
“Starting hormones early when appropriate, and staying consistent, is our best bet at reducing that risk,” Brooke explains. When started before blood vessels stiffen, proper hormone therapy can keep those structures soft and pliable, reducing the risk of clots, heart attacks, and strokes.
For me, an analogy that came to mind was of the musician. If you play the piano every day, you can maintain your skills throughout your life. If you quit as a teenager and try to pick it up again at 60, however, you won’t have stayed sharp, and your playing will be full of mistakes.
Another fear related to hormone therapy has been gynecologic cancers. But Brooke says estrogen and progesterone therapies don’t generally cause cancers to develop.
Instead, the problem occurs if a tumor exists already or develops by another means during treatment. Then, it could grow more rapidly in response to hormone therapy. Brooke shares, “I tell patients that if you stay on top of your breast imaging, and you find that there’s something concerning, we would stop your hormones or reevaluate to determine the next course of action.”
Well-Rounded Hormone Replacement: Beyond Estrogen and Progesterone
While most discussions about female hormones focus on estrogen and progesterone, Brooke emphasizes that testosterone plays a crucial role in women’s health as well. “As women, we also have testosterone, just like men have estrogen and progesterone. It’s just that we have about a tenth of what men have.”
Brooke might check testosterone levels in women experiencing fatigue, low libido, mood changes, and apathy — a loss of enjoyment in activities that once brought pleasure. For women experiencing these symptoms, testosterone replacement could be a valuable consideration.
Brooke also commonly screens for thyroid function, and she’ll check prolactin levels when patients report sudden onset of low libido, fatigue, or unexplained nipple discharge. Interestingly, she’s discovered several prolactinomas — typically benign brain tumors — through routine prolactin screening. “It’s the craziest thing to come up with, technically, a brain tumor from somebody coming in for low libido,” she shares.
Managing Expectations: The Hormone Replacement Journey
When women begin hormone replacement therapy, Brooke emphasizes that patience is essential. “Fast is not always the goal,” she tells her patients. “I know that you want to feel good immediately, and that would be lovely if I just had this magical wand.”
The process typically involves starting with modest hormone therapy and gradually adjusting based on response. Some symptoms, like hot flashes and night sweats, may improve within two weeks. Weight-related changes, however, often require three months or more to see significant resolution.
Brooke is passionate about patient involvement in decision-making and works to ensure women understand their options, such as whether to use patches, gels, or oral medications. “It just depends upon their needs and their goals,” she says. “And patients need to be involved in that decision-making.”
Otherwise, patients may not realize the type of delivery mechanism until they get home, and they may hate it. “They’re going to throw it in the garbage can,” she shares. And that won’t provide the help they need.
Looking Forward: Innovation in Women’s Health
When asked about exciting developments on the horizon, Brooke acknowledges that COVID significantly hampered medical innovation and clinical trials in women’s health. However, she’s optimistic about emerging treatments for pain management, new options for sexual desire disorders, and energy-based therapies for pelvic health.
These energy-based options — like fractional CO2 lasers, radiofrequency treatments, and electrical muscle stimulation — offer new methods for maintaining pelvic floor health and addressing various women’s health concerns. While often not covered by insurance, they represent expanding treatment options for conditions that previously had limited solutions.
Taking Control of Your Health Journey
The overarching message from my conversation with Brooke is empowering: Women don’t have to suffer through hormonal changes without support. The fear surrounding hormone replacement therapy, while understandable given the historical context, shouldn’t prevent women from exploring safe, appropriate treatment options with a knowledgeable provider.
At Brentwood MD, we recognize that women’s health encompasses far more than reproductive health. The hormonal changes of perimenopause and menopause affect every aspect of well-being — from weight management to energy levels to mood to sexual health. By understanding these changes and working with knowledgeable providers, you can take advantage of modern tools to navigate this transition with confidence and comfort.
If you’re experiencing symptoms that might be related to hormonal changes, don’t dismiss them as “just part of being a woman.” Seek out providers who understand the complexity of women’s hormonal health and are committed to finding solutions that work for your individual situation.
Your quality of life matters, and effective treatments are available when you’re ready to explore them.

Dr. Wright joined Brentwood MD in 2022 as the model allows him to spend more time connecting with patients and build a foundation of exceptional care. He is a Nashville native and completed his family medicine residency at the University of Tennessee Health Science Center, where he also served as Chief Resident. He believes that your health deserves a prominent position on your priority list, and would be honored to serve you and your family.