As a physician, I’ve seen countless patients come through my doors with a runny nose, sore throat, or persistent cough. We all have experience with these upper respiratory ailments; they’re nearly universal.
But how do you know when it’s a true upper respiratory infection vs. allergies? Or when you have a viral illness vs. a bacterial one?
Upper respiratory ailments are simultaneously simple to treat yet difficult to understand. Why? Because they have a variety of causes, yet similar symptoms! Plus, we all have our own stories, experiences, and colloquial wisdom that inform our understanding of our ailments.
Let’s discuss the reasons for the confusion surrounding upper respiratory infections, allergies, and their various treatments by clarifying the meaning behind common symptoms and identifying which treatments make sense for which ailments.
How Doctors Assess Upper Respiratory Symptoms: What Really Matters
When a patient comes to me with upper respiratory symptoms, I consider several key factors before making a recommendation. The causes of upper respiratory symptoms fall broadly into three categories:
- Bacterial
- Viral
- Allergic/Environmental
Each of these causes requires a different approach to treatment. A patient’s symptoms often point to one specific cause, but they don’t always align with popular theories about them. For example, green mucus doesn’t necessarily mean an infection; the color may only indicate how long the mucus has been present, not its origin.
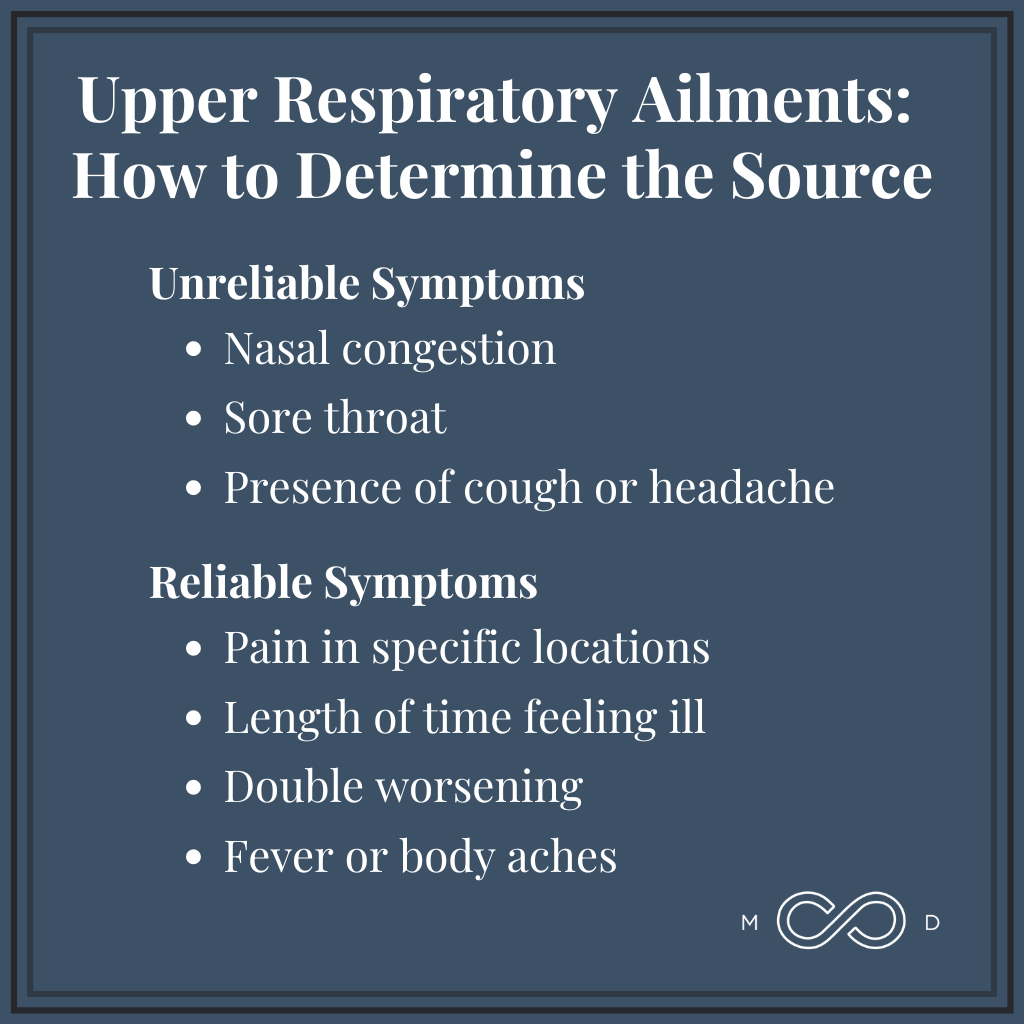
With that in mind, I categorize signs and symptoms into two lists: unreliable and reliable.
Unreliable Signs and Symptoms
Unreliable symptoms aren’t unimportant, but they don’t provide reliable insight into whether a patient has a bacterial or viral upper respiratory infection vs. allergies.
These symptoms matter very much to the patient, of course, because they get in the way of daily life. But while doctors take note of them, the following symptoms aren’t helpful for a specific diagnosis:
- Nasal congestion. As mentioned, mucus color doesn’t provide the window into health many think it does.
- Sore throat. A sore throat may stem from a bacterial infection, or it may result from allergic post-nasal drip.
- Presence of cough or headache. The existence of a cough or headache only tells us that something is amiss — not what’s causing it.
Reliable Signs and Symptoms
Other common signs and symptoms reliably help us determine the cause of upper respiratory illnesses, allowing us to recommend the appropriate treatments:
- Pain in specific locations. When patients experience pain in specific locations, such as over their right cheek or in their upper teeth, that pain offers us a clue as to the cause of the ailment.
- Length of time feeling ill. We approach treatment differently for patients who’ve felt ill for 7–10 days than for those who’ve been sick for a shorter amount of time.
- “Double worsening.” In physician speak, double worsening means feeling bad for a few days, then feeling better, and then feeling worse again. This phenomenon informs treatment as well.
- Fever or body aches. The presence or absence of fever and generalized body discomfort provide another helpful clue to doctors. As many of us learned with COVID, fever and body aches often indicate a virus that our whole body is working to fight, versus a localized bacterial infection or allergies.
Treatment Recommendations: More Than Just Prescriptions
When it comes to treating upper respiratory conditions, I often recommend over-the-counter (OTC) medications. This might seem too simple (to both patients and physicians!), but often it truly is the best course of action. Of course, when antibiotics are necessary, we prescribe those as well.
Here’s a look at how treatments differ based on the root cause:
For Bacterial Infections
Bacterial infections are the one case in which antibiotics are an effective treatment.
To determine whether an upper respiratory infection involves bacterial infection, we particularly consider the length of time symptoms have been present and whether the patient has experienced double worsening. A bacterial illness may also take longer to worsen, since bacterial infections tend to progress more slowly than viral ones.
For Viral Infections
Viruses reproduce much more rapidly than bacteria, causing upper respiratory symptoms to appear quickly. They’re also far more contagious. If a patient tells me, “My spouse was sick three days ago, and now I feel bad,” that rapid spread and onset is a clue pointing toward a viral cause.
Again, antibiotics have no effect on viral ailments. To treat this form of upper respiratory infection, we focus on giving the body the tools it needs to fight back and clear the virus on its own. These include:
- Rest
- Proper nutrition
- Hydration
- Symptom management with OTC medications
Allergy-Based Symptoms
Allergies often flare up with seasonal changes, particularly in spring and fall. Symptoms typically include watery, itchy eyes, a runny nose, and a shallow, throat-clearing cough.
For allergy treatment, we might recommend:
- OTC antihistamines like Zyrtec or Claritin
- Steroid nasal sprays like Flonase or Nasacort
- Environmental management, such as changing air filters and avoiding allergen exposure
Middle Tennessee has seen an influx of residents from places like New York and California. If you’re one of our new neighbors, you may notice seasonal symptoms you’ve never experienced before. Unfortunately, this is just a reality of living amidst a beautiful, pollen-filled landscape. I often joke that when you move to Nashville, they give you a guitar, a pair of cowboy boots, and a bottle of Zyrtec!
On a serious note, medications are only one line of defense against allergies. Strategic moves like staying inside right after the lawn gets mowed and changing home air filters can make a significant impact on symptom management.
If you can’t avoid yard work, then wearing a mask minimizes your allergen exposure. Remember, masks might have become polarizing during COVID, but people have long used them (with zero political overtones) for an effective defense against allergens.
Upper Respiratory Infections and Allergies: Final Thoughts
It’s become a common thought that patients come into doctors’ offices wanting antibiotics for upper respiratory ailments. But I think that sells patients short.
In most cases, patients don’t truly want antibiotics. They just want to feel better. If antibiotics aren’t the way to accomplish that, then with a little education and discussion, they’re usually happy to follow whatever course will get them back on their feet.
The key here is clear, thoughtful communication.
A doctor’s most powerful tool in treating upper respiratory infections and allergies isn’t their prescription pad; it’s their relationship with their patients. When physicians take time to listen to their patients and educate them with important information about their symptoms and treatments, patients are empowered to make the best decisions about their health.
Sometimes, the simplest ailments are the most difficult to talk about with clarity. But with open communication, proper education, and a tailored approach to each individual case, we can navigate these common but tricky health issues together.

Dr. Wright joined Brentwood MD in 2022 as the model allows him to spend more time connecting with patients and build a foundation of exceptional care. He is a Nashville native and completed his family medicine residency at the University of Tennessee Health Science Center, where he also served as Chief Resident. He believes that your health deserves a prominent position on your priority list, and would be honored to serve you and your family.