Download file | Play in new window |
In Western culture, the masculine experience has traditionally been defined by three core tenets: the ability to protect, provide and procreate.
Whether you agree that those criteria should be a part of our societal standards is completely beside the point. As archaic as they may sound, they’re deeply rooted in our culture, and therefore, in our subconscious.
When something keeps us from performing one of those “essential” functions, it hits us on a deeply visceral and emotional level.
This is especially true for issues around male infertility.
For those who want to procreate, any difficulty with conceiving often leads to a tremendous amount of internal stress, shame, and even conflict between partners.
Questions stack on top of questions.
“What’s the issue? Whose issue is it? How bad is it? Is there anything I can do about it? Are you doing enough on your end? Is there any hope for having children?”
And even if no difficulty has been experienced, fear of the unknown is enough to set us on edge. For example, in my own practice, I’ve spoken with many members who made the choice to focus on their professional lives first before either starting or expanding their families. But when they reach a place where they feel ready to embark into parenthood, there’s a lot of nervousness and tension around the topic.
I sat down with male fertility and men’s health specialist Dr. Matthew Pollard to discuss some of the most important aspects of male infertility.
By bringing this subject to light, I hope you can gain a new perspective on infertility and clarity around the best next steps to take if you’re experiencing issues.
What Is Male Infertility and How Common Is It?
When most people think of the term “male infertility,” we assume it refers to a man’s inability to impregnate his female partner.
But, as Dr. Pollard points out, that’s not entirely accurate. Male infertility primarily refers to the decreased likelihood of impregnating a female partner.
It’s also largely dependent on age.
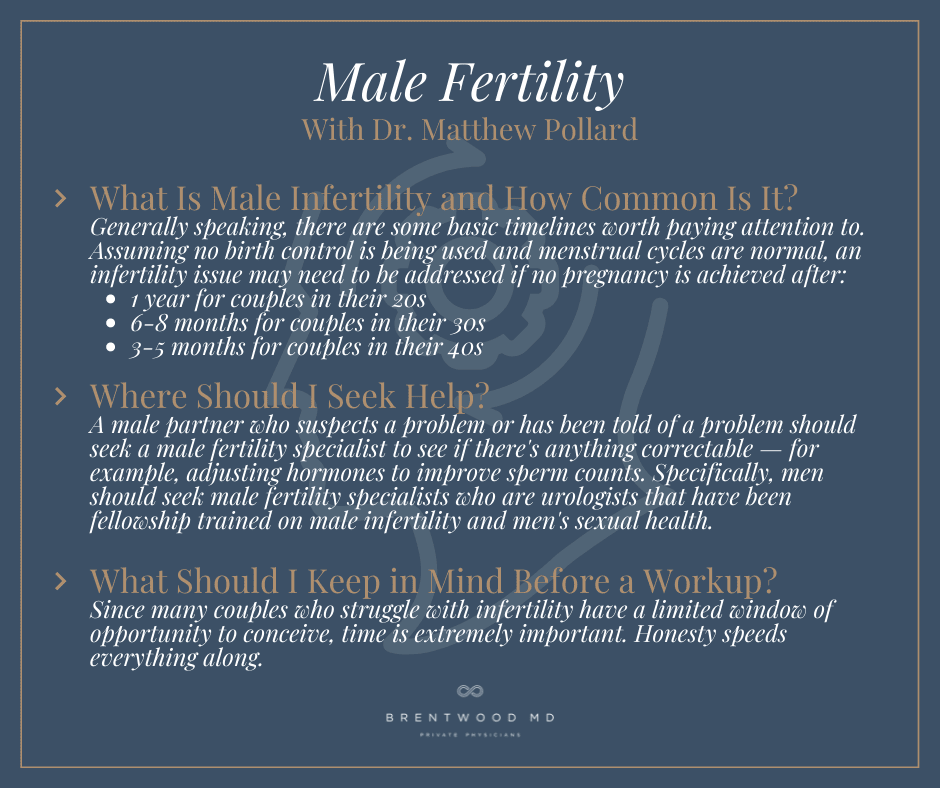
Generally speaking, there are some basic timelines worth paying attention to. Assuming no birth control is being used and menstrual cycles are normal, an infertility issue may need to be addressed if no pregnancy is achieved after:
- 1 year for couples in their 20s
- 6-8 months for couples in their 30s
- 3-5 months for couples in their 40s
No couple — regardless of their age — should expect to achieve pregnancy every cycle. While it does come faster for some couples than others, not achieving pregnancy on the first try is nothing to be alarmed about.
But if you’re unable to conceive in the timeframes mentioned above, it’s a strong indicator that you should begin having more serious conversations with the appropriate specialist.
Addressing an infertility issue can be an intimidating step for many couples — especially for the men — but it’s also more common than many people realize. Around 13% to 15% of all couples in the U.S. experience infertility issues. While it may sound small, in the medical world, that’s a highly significant percentage.
For many couples, accepting the commonality of infertility issues is very empowering. Realizing they’re not alone or statistical outliers is often enough to help them be proactive and start seeking professional assistance.
When Dr. Pollard sits down with new patients, this is one of the first points he makes.
“These conversations always start with me with telling patients, ‘This is not unusual. You’re not abnormal. This is a medical problem. More than one in ten couples experience this, and we just want to figure out what’s going on so we can help you continue to grow your family and live your happy life together.”
It’s also important to know that infertility can be caused by either partner (or a combination of both).
A common misconception is that fertility issues are primarily caused by the female. But in actuality, only about 40% of infertility issues in couples are related to the female only. Around 30% are male-only issues, and another 30% are a combination of both partners.
This statistical evenness between partners can be very enlightening for couples. By learning that nearly 60% of infertility issues involve the male, both partners realize the need to see a specialist if they suspect or experience infertility.
Where Should I Seek Help?
Even though infertility issues can be caused by both men and women, the customary gatekeepers for all fertility care have been female fertility specialists.
Traditionally, after a couple goes to their OB-GYN about a fertility concern, they’re referred to a reproductive endocrinologist (female fertility specialist). In addition to evaluating the female partner, they also usually do a semen analysis for the male partner.
If any low counts or abnormalities are present, they can refer the male to a male specialist. But that’s not always the road they take. Many times, they simply recommend exploring options for an IUI (intrauterine insemination) or IVF (in vitro fertilization).
Unfortunately, though, this does little to address the male problem that could potentially have much simpler solutions.
A male partner who suspects a problem or has been told of a problem should seek a male fertility specialist to see if there’s anything correctable — for example, adjusting hormones to improve sperm counts.
Specifically, men should seek male fertility specialists who are urologists that have been fellowship trained on male infertility and men’s sexual health.
To find a specialist in your area, visit the American Society of Reproductive Medicine and search for a provider on their directory. If none are in your area, Dr. Pollard recommends checking local urologists to see if any list credentials of a fellowship in male infertility.
What Does a Male Fertility Workup Include?
Once you decide to seek help from a male fertility specialist, the process is fairly straightforward.
First, your specialist will begin by learning your reproductive history, your partner’s reproductive history, and any history of physical symptoms or trauma.
Next, they’ll look at your lifestyle factors like smoking, alcohol intake, diet, exercise, sleep, stress and a variety of other factors that can contribute to infertility issues.
Then, they’ll conduct a physical exam and look for abnormalities like a varicocele, which can affect the quality and count of the sperm.
After the physical exam, they’ll run a semen analysis. They’ll collect a small sample and can get test results in as little as five minutes.
Beyond the semen analysis, they’ll often evaluate some basic hormones like testosterone, estradiol and estrogen, as well as several brain hormones that control testicular function.
Once they have this data, the specialist can guide you through what comes next if an issue is discovered, or what you and your partner should do if everything looks viable on your end.
What Should I Keep in Mind Before a Workup?
Again, the first thing to remember is that fertility issues are very common. Fear and shame are natural responses to infertility issues for men, but hopefully the realization that you’re not alone in dealing with this will help direct your energy in a more proactive, productive way.
Part of this means being completely honest and transparent with your fertility specialist. Concealing facts about reproductive history, past testicular trauma, and lifestyle could lead to unnecessary testing and procedures and, at the very least, delay finding a problem and its solution.
Since many couples who struggle with infertility have a limited window of opportunity to conceive, time is extremely important. Honesty speeds everything along.
Also, remember the importance of working as a team with your partner. Infertility is extremely emotional for both partners and can be a major source of conflict and tension. On the path to discovering the causes behind the issues, it’s easy to resort to blaming or judging one another.
For example, if couples discuss increasing exercise and decreasing alcohol intake with their specialist, sometimes they begin to judge one another’s behaviors and even “report them” to the specialist. But this doesn’t help the situation. Instead, be supportive of each other’s efforts to find and resolve the issues.
Should I Freeze My Sperm?
When talking about male fertility issues, we’re often asked whether or not someone should freeze their sperm.
Freezing sperm is definitely an option for men who are interested in doing it, but there are some important things worth remembering.
First, frozen sperm can only achieve a pregnancy through IVF.
Second, it can be very expensive. In addition to initial costs, there are yearly storage fees to account for.
Because of this, Dr. Pollard recommends that before contacting a sperm bank directly, let a fertility specialist guide you through the process. This way, before you commit to the large expense of freezing sperm, you can confirm that what you’re freezing is viable, high quality, and healthy.
What if I’ve Had a Vasectomy?
Vasectomies are extremely common, quick procedures performed all over the world for family planning. For men who decide they’d like to procreate after a vasectomy, there are two options.
The first is a reversal. A vasectomy reversal is a more involved procedure than a vasectomy. It takes much longer, requires general anesthesia, and must be conducted by a specialized microsurgeon.
The second option is through a testicular sperm retrieval. It’s quicker and much less invasive than a vasectomy reversal, but pregnancy can only be achieved through IVF.
Depending on your age and specific situation, a male fertility specialist can guide you through this process to choose the best option for you.
More About Dr. Matthew Pollard
Dr. Matthew Pollard is a fellowship-trained male fertility and men’s health specialist in Nashville, Tennessee. With years of urologic experience, he specializes in all aspects of men’s health, specifically male fertility, sexual health and microsurgery.
To learn more about the urologic specialties of Dr. Pollard, visit Nashville Men’s Health.

Dr. Aaron Wenzel is a concierge physician specializing in the care of fast-moving entrepreneurs, executives, and public figures in the Nashville, TN area. Dr. Wenzel’s diverse life experience and extensive training in family medicine, emergency care, nutrition, and hormone replacement therapies give him the unique platform to provide unmatched care for his patients.