Download file | Play in new window | |
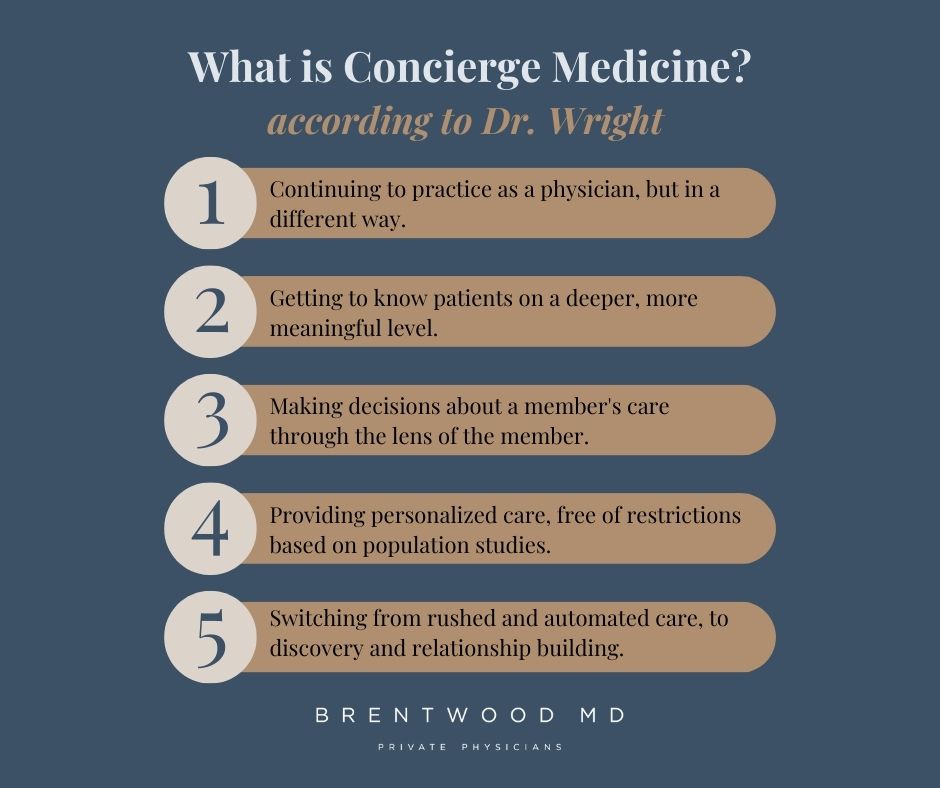
In today’s episode, host Dr. Aaron Wenzel sits down with his new colleague, Dr. Craig Wright. Dr. Wright recaps his medical journey and explains how his practice has changed since joining Brentwood MD.
After nearly a decade of practice in a traditional, insurance-based model, Dr. Wright discusses the massive transition he and his family made into concierge medicine. The switch came with challenges, realizations, and surprises — along with plenty of exciting opportunities.
Here are a few of his takeaways…
Q: What surprised you the most in your transition to a membership-based model of medicine?
The biggest surprise I had switching to a membership model was how difficult it was to explain this particular job change to friends and family.
I found myself trying to explain that I’m doing the same job. I’m seeing patients, I’m addressing wellness issues, and I’m treating illness and sickness.
But I’m doing it in such a different way that it felt new for me as a provider. I’ve also learned that it’s such a different experience for the member. It’s difficult to explain those differences unless you experience them yourself.
Through my talks with Dr. Wenzel before I joined, I was able to do some research and get comfortable with the routine and the business model, and make sure switching to membership-based care was a good career decision for me.
And now, after six short months, I’ve become bullish on this style of care as a provider — and more importantly, on this style of care for patients. I’ve told my family, “This is the only way to do primary care.”
It’s still growing, and more and more people are becoming aware of this model of care — but if we fast forward a few years from now, I believe this will be a common practice. When people consider a primary care model, hopefully, a concierge and personalized care model will be the standard.
Q: How has this transition affected the doctor-patient relationship for you?
I love getting to know people. I love getting to know their families, their work, and their priorities, so I can be useful to them as a healthcare provider. I want to give them advice that really speaks to them, and the beauty of this model of care is that there’s not a structured limit of time in routine appointments.
I’ve recognized that in a traditional setting, a patient is blessed if they’re able to get a full 30 minutes with a provider to establish a relationship. Obviously, you can still get to a certain depth in that relationship in that amount of time, but it’s rather shallow.
In hindsight, I became very good at the 10-minute sick visit and optimizing the 30-minute annual physical in a traditional setting.
There’s beauty in achieving that kind of speed while providing quality care because we need healthcare for the masses. But, as a relational person — someone who really likes to take it deeper — this switch has been beautiful for me. In concierge medicine, the doctor-patient relationship is almost what I’d consider a medical friendship.
In this case, I just happen to be a doctor, and they may or may not be a doctor. But I’ve been able to have lunch with members, and we chat about family.
At the same time, I always have what’s best for them in terms of their health, their goals, and their priorities, in mind. That enables me to chime in and be that “wise friend” who has knowledge of the health and medical world.
Ultimately, I’m able to speak to their lives in a much more deep and meaningful fashion than I ever would have in a more limited setting.
I focus on the five areas I consider to be the foundations of health: nutrition, exercise, sleep, stress management, and spiritual and relational health. And I’ve shared that for years. But now we can land there. I’ve been telling patients for years:
“Nutrition is important.”
“Exercise is important.”
But then you get back to the metrics and requirements of things you need to address in a traditional setting that may or may not be exceptionally helpful for the individual. Now, we’re able to say:
“Let’s land on these five factors and use them to tailor your care. Maybe we can even spend a whole few hours talking about just one of them because it’s clearly something you’re dealing with. Let’s go in depth.”
I truly believe those foundations are worthy of both my attention and a member’s attention. And in this model, we can truly address them, and all questions are on the table. Everybody is important, and everybody is unique.
We may have a day where we see several members, but everyone is special and has different stories. Different stressors. Different joys. Different families. Different backgrounds. And to be able to consider that in our decision-making for what’s best for their health is so beautiful, as opposed to feeling like you have to pressure the masses into a one-size-fits-all program.
Q: How has the transition affected your ability to provide excellent care?
I would say leaning into the personalization we can provide has been pertinent to providing world-class care compared to a population health approach.
I can now care for patients individually, and we’re free of many of the restrictions and checklists that are based solely on population studies. There’s obviously value in those population health guidelines and they are always considered — whether it’s a colonoscopy recommendation or a flu shot recommendation.
But we also take it to a deeper level. We get to say, “Here’s your story.” Maybe a colonoscopy needs to happen a little earlier due to your family history or certain symptoms you’ve been having. We’re able to put that population health recommendation through the lens of this individual member.
I find myself using a simple fishing analogy with many of my patients — and I’m not a fisherman! (I’d like to be, but I’m not.) When you cast out your line, you can just let your hook sit. And it can be the best cast you’ve ever done. But if you just let the hook sit, you’re never, ever going to get that fish. You’ve got to follow through, reel it back in, and go through the whole process.
If I’m explaining our model of care to a prospective member, I’m emphasizing that follow-through. I don’t want the member to feel pressure, and if the line we cast doesn’t work for them — if that strategy or goal we set isn’t attainable — that just means we need to rethink the program. Maybe we need to turn around and cast in another direction or change the bait.
That’s the beauty of this style. You’re not just throwing out lines and hoping you catch a fish. It’s about the follow-through. It’s about asking simple questions, and taking that second, third, or even fourth step. In other healthcare models, you’re limited in your ability to do that.
That’s the biggest effect I’ve seen in this care model: switching from rushed and automated care to discovery and relationship building.

Dr. Aaron Wenzel is a concierge physician specializing in the care of fast-moving entrepreneurs, executives, and public figures in the Nashville, TN area. Dr. Wenzel’s diverse life experience and extensive training in family medicine, emergency care, nutrition, and hormone replacement therapies give him the unique platform to provide unmatched care for his patients.