Download file | Play in new window | |
As a physician, I’ve noticed a trend lately: More and more patients are delaying their routine cancer screenings.
I get it. These screenings can be scary, inconvenient, and even unpleasant. But here’s the truth: They can also save your life.
Why Cancer Screening Matters
More than one in four people will receive a cancer diagnosis during their lifetime. It’s the second leading cause of death, right behind heart disease. The statistics are sobering, but here’s the good news: We have powerful tools at our disposal to detect cancer early, when it’s most treatable.
Though we would all prefer a cancer-free life, the goal isn’t just to avoid getting cancer — it’s to avoid dying from it if you do get it. And the key to surviving cancer is early detection.
This is why you hear me, my staff, and other doctors harp on and on about scheduling your cancer screenings. It isn’t to mark another box on our medical bingo cards; it’s to give our patients the best possible outcome if something is there to find.
Speed Is Everything
When it comes to cancer, especially cancers stemming from risk factors we can’t control, speed is the name of the game. Speed to diagnosis, speed to assembling a trusted medical team, speed to finding a tailored solution, and speed to recovery. But every step in this process hinges on one crucial factor: Getting eyes on the problem as early as possible.
If you don’t have eyes on the problem, you haven’t even started the race.
I understand the temptation to delay screenings due to busy schedules or fear. But consider this: There isn’t a single documented case of someone dying from stage one cancer. At that early stage, we can sometimes simply remove the cancerous cells, and you walk out cancer-free. But as cancer progresses from stage one to two to four, the five-year survival rates plummet dramatically.
Every patient I’ve encountered who discovered cancer in its later stages wishes they’d detected it sooner. The difference between stage three and stage four could mean the difference between surviving beyond five years or not. And the only variable in that equation? How quickly we found it.
Factors to Consider in Your Cancer Screening Plan
While population health gives us a general guide to the optimal times to start each type of cancer screening, your individual story provides additional factors to consider.
Age is the most significant risk factor for chronic diseases, including cancer. As we enter our fifth, sixth, and seventh decades of life, our bodies begin to malfunction. We become more likely to develop the more aggressive cancers that often yield poor outcomes, especially with a late diagnosis.
With that in mind, it probably isn’t surprising that you accrue an assortment of screenings as you pass various age-related milestones.
Family history also plays a crucial role in deciding when and what to screen. If you have a first-degree relative (a parent or sibling) diagnosed with a specific cancer, we recommend you aim to start screening for that type about 10 years before the age they were diagnosed. For instance, if your mother had breast cancer at 48, consider starting mammograms at 38 or even 35.
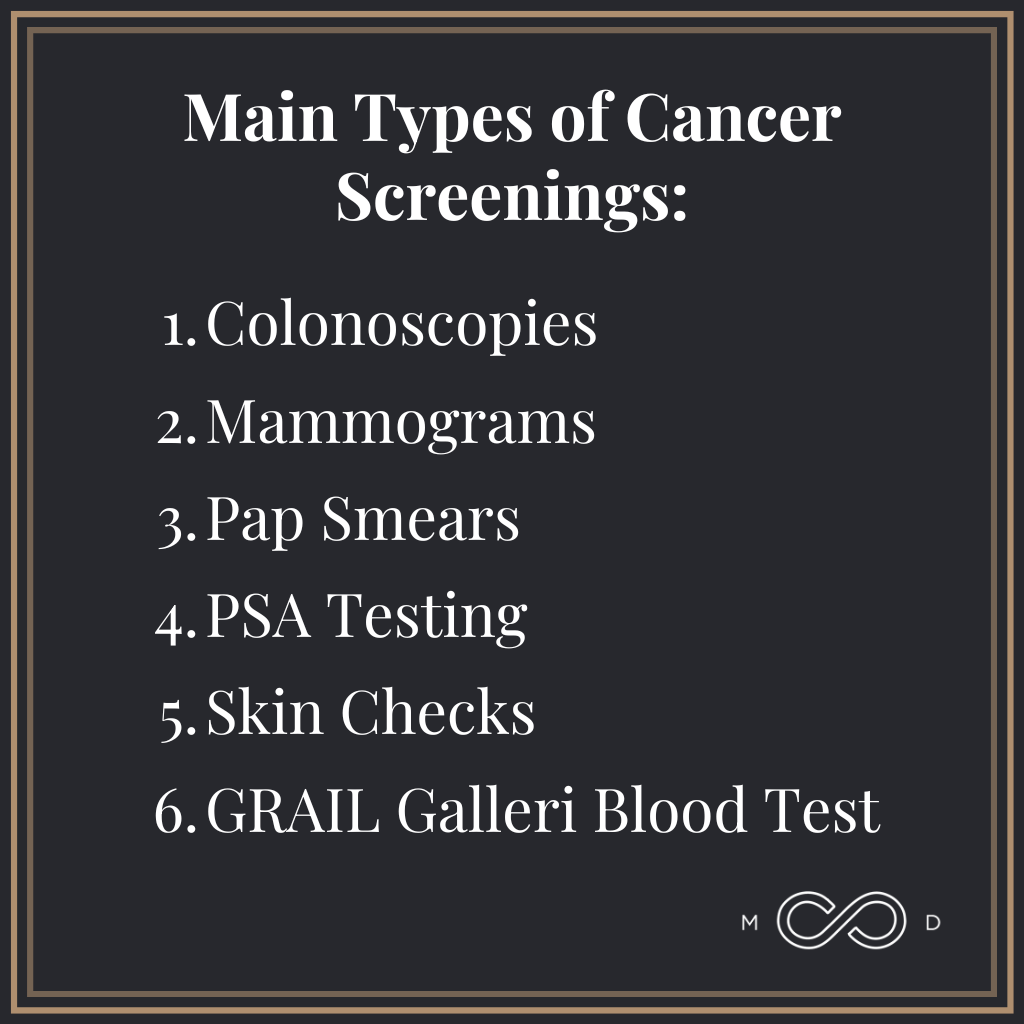
Main Types of Cancer Screenings
Today, we have regular screenings available for several of the most common types of cancer. We recommend these screenings to our members, and we suggest you speak to your physician about them, too.
- Colonoscopies: The current recommendation for starting these is now at age 45. As someone who’s had it done, I promise it’s far worse in your imagination than in reality. It’s surprisingly not a big deal, and if the results are clear, you might not need another for a decade. Bonus: This is the only cancer screening that can actually help prevent cancer in addition to detecting it.
- Mammograms: Guidelines vary, but many recommend starting annual screenings at 40.
- Pap Smears: Frequency depends on your specific situation and your doctor’s recommendations. Most organizations suggest women begin screening in their 20s.
- PSA Testing: We’re proponents of checking prostate levels (PSA) in men earlier than 50, especially for those on testosterone replacement therapy. One advantage of early screening is establishing a benchmark against which to measure any future changes.
- Skin Checks: Annual dermatologist visits are crucial, especially for those with fair skin or a family history of skin cancer.
- GRAIL Galleri Blood Test: Though not a standard screening (yet), this cutting-edge test checks for over 50 types of cancer with a single blood draw. It’s particularly effective at detecting cancers we don’t have other adequate screenings for, like ovarian, liver, and other solid organ cancers.
Combining Screening and Prevention for Optimal Health
If you truly want to live a long time and live that time well, you have to think about cancer prevention and detection. In other words, you can’t just focus on screenings and ignore a healthy lifestyle, nor can you rely solely on a healthy lifestyle without cancer screenings. Both elements are essential.
Modifiable risk factors, like smoking and metabolic dysregulation (obesity, insulin resistance, diabetes), play a significant role in cancer risk. Attacking these risk factors is one of the top steps you can take to reduce your risk of developing many cancers.
If you’re a smoker, quitting should be your number one priority this year. If you struggle with metabolic issues, talk with your doctor about strategies like intermittent fasting to reduce visceral fat and insulin resistance.
Non-modifiable risk factors involve elements you can’t change, like age, family history, and genetics. So while you go on offense against cancer where you can, it remains crucial to run a good defense with early detection through appropriate screenings.
Find Your Team
If you don’t have someone to help you navigate these decisions and hold you accountable, start there. Find a healthcare team you trust and feel motivated to be accountable to. This is your life — your only lap around the track. Dying from preventable causes is, quite frankly, tragic.
Most cases that end badly do so because we were late to diagnosis. By the time we found something, the disease had often been present for years, sometimes even a decade. It’s much more difficult to survive in these scenarios.
We have mountains of evidence and data from hundreds of millions of patients that guide our recommendations. We start there, and then we look at your individual case. So, your action plan might look just like the population health recommendations, or it may differ based on your unique challenges, family history, genetics, and symptoms.
Final Thoughts on Cancer Screening in 2024
Cancer is scary, and it’s a killer. But we have more tools than ever before to fight it, including advanced screening methods. No one wants cancer, but if it’s in your future, you want to find it as early as possible to have the most treatment options available and the best chance of beating it soundly.
We know cancer screenings bring up uncomfortable feelings for just about everyone. And it makes sense. But pushing through the sweaty palms and taking action aligns with your goal of living a long, healthy life.
A healthy dose of “paranoia” can be useful for survival. Trust your body and your lifestyle, but verify with appropriate screenings.

Dr. Aaron Wenzel is a concierge physician specializing in the care of fast-moving entrepreneurs, executives, and public figures in the Nashville, TN area. Dr. Wenzel’s diverse life experience and extensive training in family medicine, emergency care, nutrition, and hormone replacement therapies give him the unique platform to provide unmatched care for his patients.