Download file | Play in new window | |
If your goal is to live a long time and feel great, then appropriately risk stratifying your cardiovascular future has to rank at the top of your to-do list.
Heart disease unfortunately remains the number one killer of humans in the U.S. and beyond, taking an estimated 17.9 million people off the planet each year. That’s a staggering statistic, and one we’re not okay with.
For this reason, we take a little time each year to review the state of cardiovascular care, what progress has been made, and how you can take advantage of any advances in screening or treatment.
One relatively recent advance we incorporated into our practice is Cleerly, an incredible innovation in cardiac screening we’ve previously discussed on the blog. This technology changed the screening game, giving us insights into the state of patients’ heart and vascular health never before available in the history of medicine.
In this year’s cardiovascular update, the big innovation we’re reporting comes from, once again, Cleerly. We’ll dive into the details below, plus review some common blind spots to help you secure your cardiovascular future.
What Is Cleerly?
To understand what Cleerly does and why it’s so helpful, we need to take a quick look at the cause of cardiovascular disease: plaque.
Plaque begins as fatty deposits that build up along your arterial walls, causing them to thicken and narrowing the passage for blood flow. Over time, these deposits can grow, become unstable, rupture, and cause a heart attack. The other option is that they grow, remain stable, and then calcify (harden) inside your arteries.
In the past, the standard screening test was the cardiac CT calcium score, a non-invasive scan that reveals how much calcified (“stable”) plaque lurks in patients’ arteries. While this scan is useful, it can’t detect the location or amount of non-calcified (“unstable”) soft plaque — both important risk factors for your cardiac health.
Though calcified plaque is not a benign finding, it tends to be far more stable than soft, non-calcified plaque. Soft, unstable plaque can break away from the vessel wall, causing clots and blockages that lead to heart attack and stroke, often with no warning. In other words, the first sign of cardiovascular disease involving soft plaque could be sudden death.
Enter Cleerly.
Cleerly measures the entire plaque burden — both calcified and non-calcified — in the coronary arteries, allowing us to better assess risk and treatment options for patients.
To get a Cleerly scan, patients visit a local imaging center for a cardiac CT. We then upload the CT result to Cleerly’s AI-driven portal, which analyzes the images and extracts granular data about the nature, amount, and location of plaque present. It then provides us with a detailed report — including high-resolution images — of a patient’s risk level, which helps us determine the next steps for managing or treating cardiovascular disease.
A Step Further: Cleerly’s Latest Innovation
Just this year, Cleerly added a new feature to its cardiac screening repertoire. The tool, Cleerly ISCHEMIA, predicts the likelihood of ischemia in patients with coronary artery disease.
Ischemia refers to an inadequate supply of blood (and therefore oxygen) to part of the body. As you can imagine, this is a dangerous situation for your heart.
Cleerly’s ischemia predictor uses a complex combination of extensive data, AI, and other factors to determine the likelihood of ischemia in a person’s blood vessels. And, according to at least one clinical trial, it does so more accurately than existing (and more onerous) testing methods.
Besides the mind-boggling level of individualized medical insight, one of the most attractive aspects of Cleerly’s ISCHEMIA tool is its simplicity. Patients don’t have to do any additional or invasive testing; they just need a Cleerly scan. Their physician simply puts in an additional order for the ischemia prediction.
Who Needs Cleerly and When?
In general, we recommend average-risk people consider a baseline Cleerly scan in their early 50s to establish a baseline. Those with a family history of heart disease or concerning personal markers, such as high cholesterol or high blood pressure, may want to get one sooner.
Anyone who has an interest in and concern for their cardiovascular health can certainly consider a Cleerly scan just to make sure they aren’t missing anything.
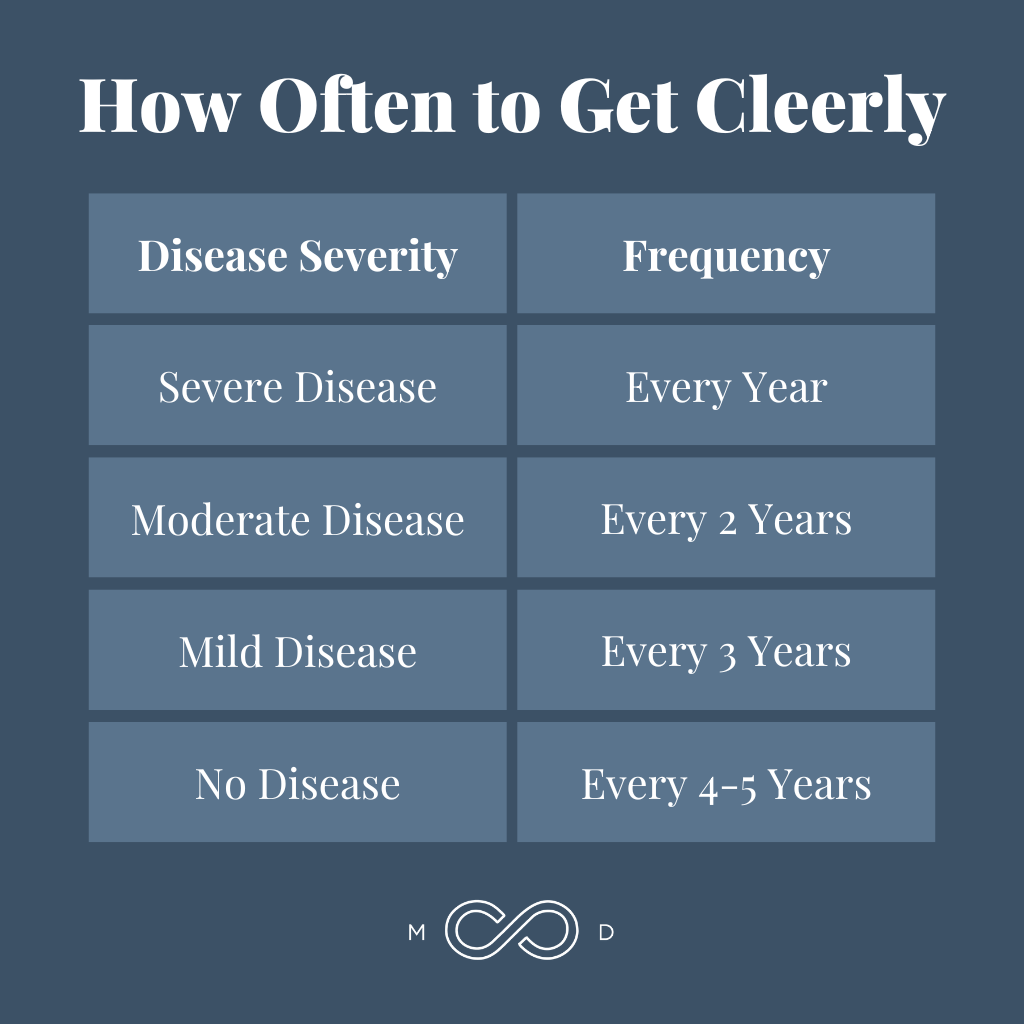
The frequency of follow-up scans depends on your initial results:
- Severe disease — every year
- Moderate disease — every 2 years
- Mild disease — every 3 years
- No disease — every 4–5 years
Of course, cost is always a consideration. If you have symptoms that would warrant a CT scan anyway, your health insurance may cover the CT portion of the screening. In most markets, this ranges from several hundred to $1,000.
The Cleerly analysis portion of the process is an out-of-pocket expense, typically ranging from under $1,000 to around $2,000 depending on a range of factors. For example, we work hard to ensure our members don’t have to make separate cardiologist or internist appointments just to get their Cleerly scans.
While we realize the cost isn’t insignificant, we believe Cleerly is a worthwhile investment to get eyes on one of the most significant factors involved in your health and longevity.

A Clearer Path Forward
One of the most powerful aspects of Cleerly is that it enables truly personalized and informed decision making. No more guessing games or one-size-fits-all algorithms.
With Cleerly, we can see the actual state of your arteries and have an honest discussion about next steps, whether that’s dietary changes, medications, or both. It gives us confidence that our approach is perfectly tailored to your specific situation.
We’ve been using Cleerly with patients for several years now, and we can say without exaggeration that it has saved lives. Even for patients who were nervous about getting the scan, it often provided the wake-up call and motivation they needed to finally take action.
For example, one patient recently received Cleerly results that showed moderately worrisome findings. It wasn’t the news he wanted, but it was exactly what he needed to start making changes.
Sometimes, we have to suffocate excuses with truth. There’s nothing quite like looking up at pictures of your coronary arteries with your physician and hearing a detailed report. With the truth right in front of you, the question becomes not, “Do I really need to make a change?” but “What am I going to do about this very real situation?”
All progress begins with telling the truth. In my experience, I’ve found that most free-thinking, intelligent humans are capable of making uncomfortable decisions when presented with the truth.
Go Blind Spot Hunting
While Cleerly is an incredible screening tool, providing insight into previously unknowable aspects of your health, screening only tells you the state of things. It doesn’t divulge how they got that way or what to do about them — though it can provide incredible motivation to do something.
Besides taking advantage of Cleerly, the greatest area of opportunity for you to make a meaningful impact on your future heart health is in addressing what I call cardiovascular blind spots.
Blind spots are factors that significantly influence heart health but that many people aren’t aware of. When we get our eyes on these factors and give them an appropriate amount of attention, we can make a real impact on our cardiovascular futures.
Blind Spot 1: Metabolic Disease
Outside of not smoking, metabolic disease is the number one blind spot when it comes to heart disease (not to mention dementia, cancer, and more). Currently, the societal tendency is to sleep on metabolic disease until it becomes something we can’t ignore — like diabetes.
The following are three metabolic factors we need to monitor and address if we want to manage cardiovascular risk:
Insulin Resistance and Diabetes
Insulin resistance and diabetes are by far the most common and concerning metabolic blind spots I see with new patients.
Diabetes doesn’t just appear out of nowhere — it develops slowly over years and decades, often with warning signs 5, 10, or 15 years before full-blown disease sets in. When we ignore these signs, we set ourselves up to develop one of the biggest potentially avoidable cardiovascular risk factors there is.
So today, if you don’t have a crystal clear picture of your metabolic health and insulin sensitivity, stop what you’re doing and figure that out.
To learn more about how to address and assess your status, take a look at our previous posts: Enemy #1 — Metabolic Disease and Can You Reverse Metabolic Syndrome?
Visceral Fat and Waist Circumference
Truncal obesity, or excess visceral fat in your abdomen, is one of the most dangerous yet overlooked risk factors for cardiovascular disease. This isn’t about love handles or a few extra pounds — it’s about fat accumulating around your internal organs.
Measuring your waist circumference is a simple way to track visceral fat. As you shrink your waistline, you directly improve your metabolic health and reduce your all-cause mortality risk.
Hypertension
Hypertension, or high blood pressure, is one of those factors we can easily overlook because it doesn’t typically cause symptoms. Whether it’s failing to treat hypertension or failing to treat it to goal, we often miss the mark.
I’m personally guilty of this, ignoring my mild hypertension until a Cleerly scan showed that even “borderline” high blood pressure takes its toll on the arteries. Now that I understand the risks, I take all hypertension very seriously in myself and my patients.
Blind Spot 2: Sleep Apnea
Untreated sleep apnea is another common blind spot that significantly increases cardiovascular risk. As it turns out, properly oxygenating your body through the night is crucial for heart health.
If you snore, or if your partner says you snore, please get a sleep study to check for apnea. It’s a far more dangerous risk factor than many people realize and relatively simple to treat; don’t ignore it.
Blind Spot 3: Advanced Lipid Testing
It isn’t shocking that most patients haven’t heard of the following two blood tests. Even many doctors in conventional, insurance-based practices aren’t familiar with them.
Though few people test for them, these are the two most important markers in blood work for cardiovascular risk:
Apo B or LDL Particle Number
Apo B, or LDL particle number, is much more predictive of cardiovascular events than typical cholesterol measures. Ask your doctor to check your Apo B or LDL-P and track it over time. Make sure you understand your results and take steps to optimize them.
Lipoprotein(a)
Elevated levels of lipoprotein (a), or Lp (a), can significantly increase heart disease and stroke risk, independent of other cholesterol markers.
Lp (a) levels are largely genetic. While you can’t change your genes, knowing your Lp (a) status allows you to manage that risk more aggressively. Don’t let yourself remain blind to this powerful, yet often ignored, risk factor.
How to Take Action
Sometimes starting can be the hardest part. If you aren’t sure what to tackle first, we recommend working through the following:
- Find Your Team. The first step is to find a physician you trust to be your partner in cardiovascular health. Look for someone who’s knowledgeable about the complex matter of cholesterol, who understands tests like Apo B and Lp (a) and what to do with them.Not knowing about Cleerly or Apo B and Lp (a) isn’t a crime. What becomes a crime is being unwilling to listen or have a conversation. If your current doctor isn’t the right fit, ask for recommendations from friends or do a quick online search to find a physician who will be in your corner.
- Know Your Numbers. You can’t manage what you don’t measure. Make sure to track key health indicators like blood pressure, metabolic profile (fasting insulin and glucose), lipid panel (including triglyceride to HDL ratio), Apo B, and waist circumference. Stay on top of whether these numbers trend up, down, or remain stable over time.
- Don’t Ignore the Borderline. Don’t brush aside borderline diagnoses like pre-diabetes or mild hypertension. In reality, “borderline” just means “early disease.” Borderline is, in fact, the best time to take action because it affords the greatest chance to reverse the problem before irreversible damage occurs.
- Consider Adding Cleerly. While it requires an investment, the Cleerly scan provides unique insights into hidden cardiovascular risks that can be lifesaving. Discuss with your physician if Cleerly makes sense for you as part of a proactive prevention plan. Visit cleerlyhealth.com to learn more about this advanced testing option.
The stakes couldn’t be higher, but you have more tools and insights at your disposal than ever before. It’s never too late to take action. Get started today.

Dr. Aaron Wenzel is a concierge physician specializing in the care of fast-moving entrepreneurs, executives, and public figures in the Nashville, TN area. Dr. Wenzel’s diverse life experience and extensive training in family medicine, emergency care, nutrition, and hormone replacement therapies give him the unique platform to provide unmatched care for his patients.






