Download file | Play in new window | |
This month, my podcast copilot Jen Justus and I talk about a modern-day epidemic. It’s a disease that’s become so common in the United States that we’ve almost normalized it — a dangerous development that keeps us from talking about just how harmful this disease is.
The disease we’re talking about is obesity.
And yes, obesity is classified as a disease. Obesity is probably the single most important topic in primary care medicine, and it also happens to be the origin of Jen and my practice together. We’ve learned so much about weight-related diseases over the years, and we’re excited to share a state-of-the-union update with you about where we are collectively in the battle with obesity.
What Is Obesity?
If you’ve struggled with your weight, you’re not alone. According to the Centers for Disease Control (CDC), three-quarters of the U.S. adult population is overweight, and over 40% is obese.
The CDC defines obesity as a body mass index (BMI) greater than 30. Your BMI is your weight in kilograms divided by your height in meters squared — but unless you love math, you can just use an online BMI calculator to get your number.
It’s important to note, though, that BMI is a screening tool, not a diagnostic tool. It doesn’t account for what makes up your body mass, only how much of it there is relative to your height. So body builders get flagged as obese even though they actually have very low body fat, and a thin person can fall into the “healthy” range on the BMI chart, but have a high percentage of body fat.
So why even look at BMI? While less useful on an individual level, BMI becomes more important at a population level. Yes, there will be exceptions, but not a significant number above a measurement of 30 or so. At that level, BMI tells us fairly accurately how we’re doing as a collective, and whether we’re mapping in the right direction.
To be clear, obesity isn’t about appearance. It’s about the health risks that come from carrying too much fatty tissue on your frame, especially in your torso.
DOWNLOAD OUR FREE EBOOK
Concierge Medicine is the future of healthcare.
Learn more about this refreshing alternative to traditional primary care, and decide if it's right for you.
Key Considerations to decide...
Is Concierge Medicine Right for You?
Metabolic Disease and Metabolic Syndrome
The reason we’re interested in BMI as an indicator of obesity is that obesity is a significant red flag for one of the dangers Jen and I talk about most — metabolic disease.
If you’ve heard some of our other episodes, you’ll recognize the term metabolic disease. We feel strongly about metabolic disease and want to sound the alarm on just how serious it is.
Metabolic disease occurs when you have an abundance of potential energy stores in your body. It’s an excess energy state, or energy dysregulation, during which we constantly store energy (fat) but never burn it off.
Metabolic syndrome is a group of conditions that raise your risk for diseases like heart disease and diabetes. You’ll receive a diagnosis of metabolic syndrome if you have three or more of the following five risk factors:
- Waistline greater than 40 inches for men and 35 inches for women
- Elevated triglycerides
- Low HDL cholesterol
- High blood pressure
- Elevated fasting glucose
Though it’s rarely talked about, the root physiology behind metabolic syndrome is insulin resistance. It’s the underlying influence that leads to all these other risk factors, lurking for years beneath the surface before it eventually manifests as serious disease.
So why does being obese matter? It puts you at high risk for metabolic diseases, which pour lighter fluid on the flames of many of humanity’s top killers, including diabetes, heart disease, cancer, and dementia.
This is THE health issue in humanity right now, increasingly even among children. No disease will outpace diabetes in the next 20 years worldwide. It’s time for red lights and sirens. We could get everything else right, but if we miss this, we’re not going to make a significant impact on the health and well-being of our species.
Why ‘Eat Less, Exercise More’ Is Not the Answer
Why have we failed to successfully address obesity? The old approach was to tell people to eat less and exercise more. That sounds simple enough. But if it was that easy, why have our obesity rates continued to increase?
Let’s look at three facets of the old way of addressing obesity and why they haven’t worked.
The Old Way #1: All Calories Are Created Equal
Historically, the most fundamental thought related to weight loss was the myth that “all calories are created equal.” But this simply isn’t true.
It all goes back to understanding biochemistry and how the types and qualities of food you consume affect your blood sugar and insulin — your fat-storing hormone. If all calories were created equal, then eating 100 calories in Oreos would be the same as eating 100 calories in broccoli. But these foods produce different hormonal, metabolic responses in our bodies. We know intuitively that they aren’t equivalent, but the calories-in-calories-out philosophy has overridden instinct for years.
“Calories in, calories out,” has been prescribed as the one-size-fits-all, universal weight loss solution for every person on the planet. Eat less. Exercise more. But look where that’s gotten us.
Weight loss isn’t just a math problem. You can’t simply outrun your mouth. Math is a variable, certainly, but weight loss is far more a biochemistry and hormone balance problem than it is simple substraction. We have to recognize that if we’re going to make meaningful progress in metabolic health.
The Old Way #2: What vs. When
The second problem has been an intense focus — almost a religion — on what we eat rather than when we eat.
We’re not saying that what you eat isn’t important. It is. But we’re saying that the focus is misplaced. As a practitioner in this space, I have no doubt that when you eat is THE most important factor in weight management.
People debate about what to eat constantly, and there’s always another diet, another fad, and another fizzle. But until recently, very few people asked the higher order question of when you should eat that food.
Part of this comes from a convergence of Venice Beach body-building culture of the ’60s and ’70s, bro science, and mass agriculture all selling the idea that we need to eat every two or three hours as humans, which is nonsensical. In the history of humanity before 1900, we rarely ate more than one meal a day. Humans simply aren’t designed to live in all this abundance.
Many mainstream diets stress the importance of eating three meals a day. Even worse, some advise eating five or more small meals throughout the day. And don’t even think about skipping breakfast.
This has created a metabolic disaster. The result is insulin resistance and metabolic disease.
The Old Way #3: Normalizing Disease
The third approach that’s gotten us into trouble is normalizing metabolic disease. We haven’t talked too much about this factor before, but it really weighs on me.
Normalizing obesity and metabolic disease may come from a desire to be kind, inclusive, and caring. We don’t want to hurt people’s feelings, or make them feel less. But in our effort to be loving and supportive, it’s possible that we stop telling the truth, because the truth is hard.
All progress begins with telling the truth, and we’re not being truthful about a disease called obesity.
When we normalize it by saying things like, “You’re just big-boned,” or “You’re beautiful the way you are,” we’re ignoring that obesity has nothing to do with a person’s worth, value, or beauty. It has everything to do with living in a disease state that reduces their quality of life and shortens their length of life.
Obesity is not about appearance, and we have to be honest about it. We can be honest with kindness and provide resources and support to people who are struggling. But normalizing the problem will only make it worse.
One term I’d love to see disappear from our medical vocabulary is borderline. If a doctor tells us, “You’re borderline obese,” as human beings we think, “Great, I’m not obese.” Borderline is deadly because it normalizes the condition. In reality, there’s no such thing as borderline. There’s just early disease. Early heart disease. Early diabetes. Early hypertension. You haven’t dodged a bullet; you’re getting lined up in front of the target.
If you receive a diagnosis of borderline anything, it’s a sign that you need to take immediate offensive action to reverse your condition before it’s too late.
The Brentwood “Old” Way
At Brentwood MD, we’ve implemented so many new ways of approaching weight loss, from focusing first on the timing of meals to hunting for metabolic disease on day one. We then focus on the quality of what our patients eat and potentially carbohydrate restriction or calorie restriction if necessary. We work on optimizing fitness plans, improving sleep hygiene, modifying alcohol intake — whatever each individual needs to be successful.
We strive to stay innovative in delivering handcrafted strategies. We don’t jump onto every new trend, but when something shows legitimate promise, we’re at the front of the pack in examining the data and putting new tools into practice.
A New Breakthrough in Weight Loss
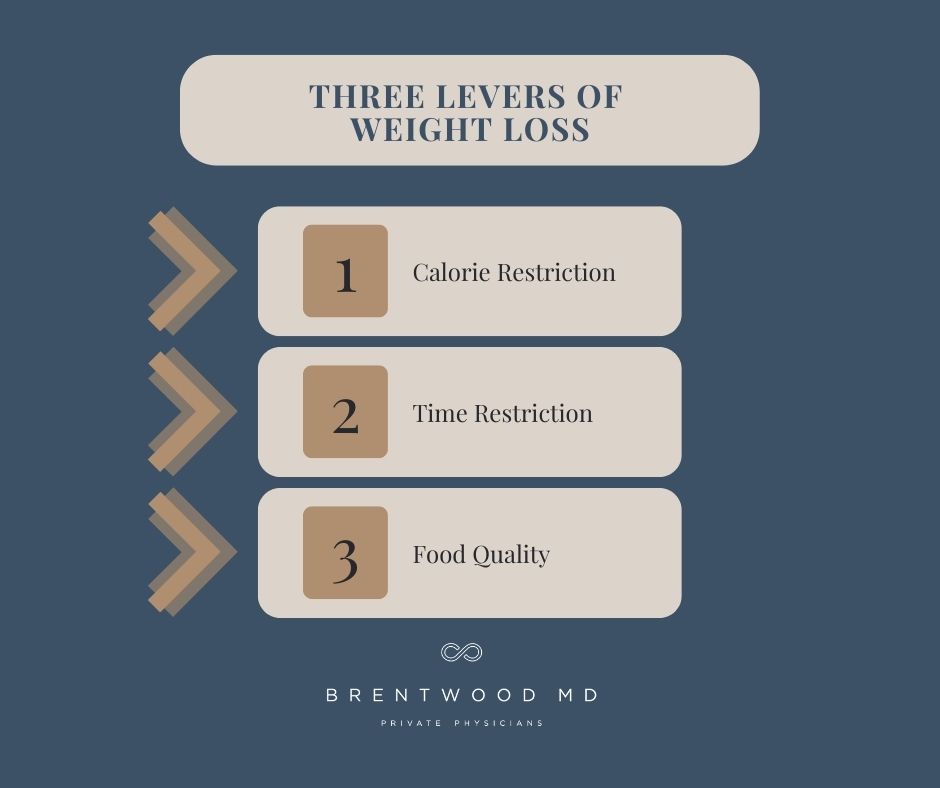
We’ve been following our new way of treating obesity for a long time. We have a ton of content discussing intermittent fasting and why diets don’t work. In our consideration, there are three levers that people can pull to manage their weight: calorie restriction, time restriction, and food quality. To avoid gaining weight, all humans have to pull at least one of those levers at all times. To lose weight, you have to pull at least two levers at once.
Lever 1: Calorie Restriction
Though we don’t subscribe to the notion that all calories are created equal, we do recognize that people need a calorie deficit to lose weight. This is caloric restriction, and it’s hard.
Limiting the amount of food you eat can be exhausting. Add calorie-math on top of that, and it’s not hard to see why this is the least-reliable lever in terms of practicality and adherence. Because of this, calorie restriction isn’t usually the option we turn to first.
Lever 2: Time Restriction
We’ve found time restriction, or how often you eat, to be the most powerful lever by far. By focusing on restricting your eating window, you can improve your body’s insulin sensitivity, avoiding metabolic disease.
For most of our members, we suggest delaying breakfast and just eating two meals a day of whole food, eating to satiety, with no snacking in between. Start your fasting window after the last thing that goes in your mouth in the evening, and then just start up about 16 hours later. Many people find this much easier than they imagine.
Lever 3: Food Quality
As we mentioned earlier, the quality of the food you eat matters in your weight loss goals. Substituting whole foods and macronutrients for processed and junk foods will make a big difference in your progress. This is the second lever we recommend pulling if time restriction alone isn’t making the difference you want to see. Particularly, reducing carbohydrate intake is often an effective strategy, given the relationship between carbohydrates, blood sugar variation, and insulin resistance.
 A Game Changer in Weight Loss
A Game Changer in Weight Loss
In 2005, a new class of medication called GLP-1 inhibitors hit the market as a treatment for type 2 diabetes. GLP-1 (glucagon-like peptide 1) inhibitors act at the level of your gut to affect insulin secretion, food digestion, and appetite. They even slow the process of gastric emptying, meaning food sticks around in your stomach longer so you feel full with smaller amounts of food for greater lengths of time.
This has an extremely beneficial impact on diabetes, but we’ve also found that it has a favorable side effect for non-diabetics: weight loss. The most common GLP1 drug names are:
- Dulaglutide (Trulicity)
- Exenatide (Byetta)
- Extended-release exenatide (Bydureon BCise)
- Liraglutide (Victoza)
- Lixisenatide (Adlyxin)
- Semaglutide (Ozempic, Rybelsus, Wegovy)
Some of the most common side effects are gastrointestinal symptoms like diarrhea, nausea, constipation, bloating, indigestion, and headache. However, because the dosing of these drugs is very subtle, we don’t see a lot of side effects that people find intolerable or overly disruptive in daily life.
One of the only issues we run into with GLP-1 inhibitors is that they can be expensive, sometimes upwards of $1,500 per month, and insurance does not cover them. However, there are cost-savings programs available that some people can enroll in for assistance.
The other disadvantage is that GLP-1 inhibitors are typically administered via injection, which can be an issue for people who can’t stand needles — though these needles are tiny and easy to use.
GLP-1 inhibitors have proven so effective and so well-tolerated for weight loss that the FDA has now approved several for weight loss in patients without diabetes. This is a huge breakthrough for people who have been pulling all the levers but still struggle to lose weight.
Action Steps for Obesity
If you struggle with obesity, don’t give up. You’re not alone, and you can make progress. Try these practical steps to get started.
First, find your team. By “team,” we mean a group of healthcare professionals who create an environment where you’re free to have open conversations about all the options and what’s best for you. If you don’t have that already, start looking for this today.
Second, find out what intermittent fasting means for you. Maybe start by skipping breakfast and not eating after 8 p.m. Gradually try to extend your fasting window beyond 12 hours.
Third, find another lever you feel comfortable pulling. Maybe counting calories makes the most sense for you. Or maybe cutting carbs will help. Whichever one you choose, make a commitment to it.
If you’re pulling levers and nothing seems to help, talk to your team about whether a GLP-1 inhibitor might be a good option for you. It could be the key that unlocks weight loss for you.

Dr. Aaron Wenzel is a concierge physician specializing in the care of fast-moving entrepreneurs, executives, and public figures in the Nashville, TN area. Dr. Wenzel’s diverse life experience and extensive training in family medicine, emergency care, nutrition, and hormone replacement therapies give him the unique platform to provide unmatched care for his patients.