Did you know that your body only has one mechanism to lower blood sugar, other than exercise?
Insulin.
But what happens when that one mechanism begins to fail?
In today’s blog, we’re going to unpack the concept of insulin resistance. I believe it is one of the most important and critical topics in all of medicine for the next 20 years.
In fact, I would go so far as to call optimizing blood sugar the holy grail of health.
To Be Diabetic Is to Be Insulin Resistant
Most people think you just wake up one day with diabetes. This is just not the case.
Diabetes is actually a continuum or spectrum. This means that you become diabetic over the course of five, ten, or fifteen years.
The spectrum begins with mild insulin resistance that progresses to a blood sugar of 126, or seven teaspoons of sugar in your bloodstream — just two teaspoons of sugar above a non-diabetic.
In order to understand insulin resistance, we first need to answer some critical questions.
What Is Blood Sugar?
Blood sugar is a mechanism by which we deliver fuel or energy to our body so that we achieve the primary goal of all living things, which is to stay alive.
Blood sugar is energy.
Why Is Sugar Such a Big Deal?
It’s a big deal because sugar is the simplest, most readily available form of energy that our body uses to keep us alive.
Once our blood sugar hits a level of 100, or five teaspoons of sugar, the body begins to store the rest as fuel for later. This accomplishes two things: It helps us to survive famines in the future, and it also gets sugar out of our bloodstream before the amount reaches seven teaspoons, which is the level of diabetes. So, your body avoids wasting sugar while skirting a diabetic blood sugar level in the process by pushing all that excess sugar into fat.
One intermediate step is all it takes to collect sugar and drive it into a fat cell. This is hugely important.
How Does Insulin Resistance Occur?
In order to answer that, we need to understand “normal” first. In other words, what does our body normally do by design in the presence of elevated blood sugar? When your blood sugar rises above 100, a signal is immediately sent to your pancreas to release the hormone insulin.
Insulin does two things — it lowers blood sugar by driving it into the cells, and it converts sugar into fat.
So as blood sugar normalizes, the insulin goes away entirely. Then you have this relationship in a normal scenario: sugar rises, insulin rises, sugar falls, then insulin falls.
This is normal.
Over time, as blood sugar remains elevated even in the presence of insulin, the body releases even more insulin to correct the high blood sugar, and then your blood sugar drops. But our body starts resisting insulin, which results in chronically elevated blood sugar.
The More Insulin Resistant You Become, the Higher Your Blood Sugar and Insulin Levels Become
This is the basic premise of insulin resistance.
But why is this a big deal?
Insulin resistance is a chronic progressive disease, which means if left alone, it not only doesn’t go away, it also gets worse. And eventually, our blood sugar becomes so elevated that we are diagnosed with diabetes.
This is how tightly our body controls blood sugar. It’s super important to be alive but we want no extra because we don’t want diabetes.
Diabetes Is a Progression of Insulin Resistance
You are profoundly insulin resistant with diabetes as opposed to mildly insulin resistant with pre-diabetes.
An out-of-control diabetic is also insulin resistant, they’re just out of control. They have an inability to respond to any level of insulin that their body is able to produce.
And what happens to those people when they go to the physician? What does your doctor put you on when your pancreas is working overtime and you can’t produce enough insulin to get that sugar down because your body is ignoring it?
You guessed it — MORE INSULIN.
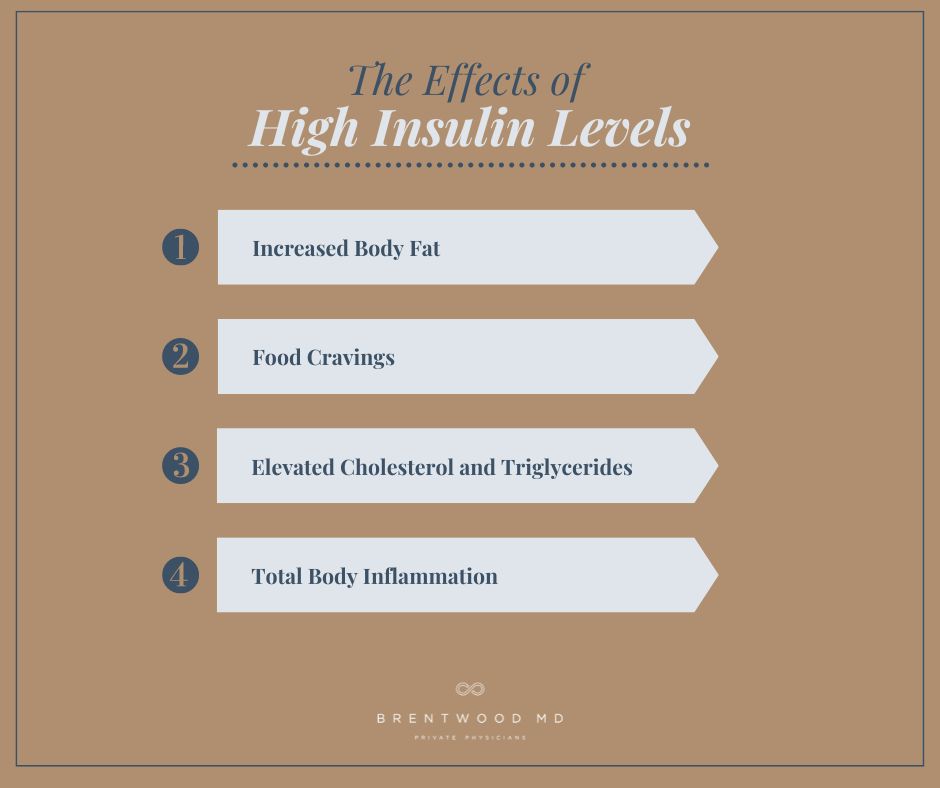
The Effects of High Insulin Levels
Elevated insulin is a big deal because it does a number of horrific things.
1. High Levels of Insulin Make You Fat
Insulin is a fat-making hormone.
At high levels, it blocks you from ever being able to burn fat. Even if you are working out and sweating every day, if your insulin levels are still high, you won’t burn fat. If insulin is present, you are not burning fat; you’re making it.
You’ve got to normalize your blood sugar to lower insulin levels. If your body’s ignoring the only mechanism to get that blood sugar down, you’re going to be in trouble.
By adopting healthy lifestyle habits, including a diet for insulin resistance, moderate exercise, and improved sleep, you can reduce body fat and regulate insulin levels.
2. High Levels of Insulin Cause Cravings
Insulin triggers the craving center in your brain. Think about it — if insulin is related to blood sugar, what do you think insulin makes you crave? Sugary foods. Carbohydrates.
This is why people with diabetes are always hungry.
And don’t think that switching to diet soda and sugar-free candy and treats will help you beat this. Studies show that diet soda and sugar-free foods can actually increase cravings for sugar, resulting in weight gain — which exacerbates insulin resistance.
3. High Levels of Insulin Raise Bad Cholesterol and Triglycerides
The American College of Cardiology proposes that having diabetes is a risk equivalent to having established heart disease.
Insulin stimulates your liver to overproduce bad cholesterol, suppresses your good cholesterol, and increases your triglycerides.
When cholesterol accumulates in your bloodstream, it puts you at a much greater risk of developing heart plaques. Atherosclerosis, the hardening of arterial walls by plaques, develops. The plaques that harden can break loose and travel through the bloodstream.
This is a heart attack or stroke waiting to happen.
For more information on understanding cholesterol and how it impacts your health, check out this article.
4. High Levels of Insulin Increase Total Body Inflammation
Why does total body inflammation matter? Because inflammation is at the root of every disease known to mankind — arthritis, chronic pain, acid reflux, Alzheimer’s, dementia, stroke, and cancer.
The inflammatory process that takes place in the presence of elevated insulin is severe. When you’re in a state of constantly elevated insulin, you are chronically inflamed. Allergies, rashes, joint pains — it just never ends.
When you get control over your insulin and decrease total body inflammation, you improve your overall health, well-being, and longevity. This could literally add quality years to your life.
How Do You Know if You Have Insulin Resistance?
There are some early signs to look for.
1. Slow Rise in Blood Pressure
This is often due to the pro-inflammatory state. We start seeing increases in the blood pressure top number, the systolic, above 135. There may be no other symptoms, but this rise in blood pressure is suspicious, and it’s one of the earliest signs that we see.
2. Increased Belly Girth
Insulin deposits fat along the waistline. For men, waist measurements greater than 40 inches are at a higher risk of developing type 2 diabetes. For women, that number is 35 inches. Keep in mind this is a guideline and for some people, that number could be less.
Increased belly circumference directly correlates with an increase in all causes of mortality, including heart disease and cancer.
3. Change in Cholesterol Numbers
Typically, we see bad cholesterol (LDL) go up, along with triglycerides. We also see good cholesterol (HDL) go down. These are all indicative of early insulin resistance.
4. Increased Fasting Blood Sugar
This is a later finding.
Fasting blood sugars begin to rise from 85 to 90, 90 to 95, 98, 105, and 109. Yet you’re still being told “Oh, don’t worry. You’re not diabetic.” Yeah, but 126 is diabetes!
This is a huge disconnect.
If You’ve Been Told You’re Borderline Diabetic, You’re Definitely Insulin Resistant
Some other warning signs that your insulin resistance is progressing are chronic fatigue, an increase in cholesterol levels that require statins, low thyroid levels, and low free testosterone levels (male and female).
The good news is that with changes in diet, exercise, and sleep habits, you can reverse these effects and decrease insulin resistance.
Conversations to Have With Your Physician About Insulin Resistance
1) Am I Insulin Resistant?
The first step to answering this question is to find a physician who knows what this means and how to diagnose it. Finding a physician who understands is everything.
Generally speaking, your physician needs to test you for those early indicators we talked about — cholesterol, blood pressure, and obesity.
- Have them check your total cholesterol panel to see if your bad cholesterol is elevated and your good cholesterol is low.
- Have them check your blood pressure to see if it is starting to rise — usually 135/80 or greater.
- Have them look for truncal obesity. In other words, you’re getting heavy around the belly.
These are all very, very telltale signs that insulin resistance is at play.
2) If I’m Insulin Resistant, How Do I Treat It?
There are really only a few ways to treat insulin resistance.
Diet — First and foremost, you need to make radical diet changes to avoid elevated blood sugar and elevated insulin.
Focus on cutting out sugary drinks like soda and sweetened tea or sugar in your coffee. Food and drinks that are high in sugar promote insulin resistance. Try to eliminate highly processed foods like snacks or convenience meals. If you eat a lot of fast food, try to cook at home more.
Focus on eating more fresh meats, fish, fruits, and vegetables. Not only are these lower in sugar than processed meals, they also contain important vitamins, minerals, and fiber that keep you healthy and help stabilize your blood sugar.
Changing your diet helps by minimizing or eliminating the things that raise your blood sugar. It also gives your body a chance to recover the mechanism God gave you — insulin — that your body has been ignoring.
You’ve got to fix your diet, but remember: the best diet for insulin resistance is the one that you stick with. Make sure it’s not a crash diet that will end up doing more harm than good. Change your habits and make sure your diet fits well with your lifestyle so that you are more likely to stick with it in the long run.
Exercise — The best way to lower your blood sugar is to not eat things that raise your blood sugar. But presupposing you find a way to consume something that raises your blood sugar, you’ve only got two ways to lower blood sugar — insulin and exercise.
Using your muscles to exercise consumes and burns free sugar and increases insulin sensitivity by reversing insulin resistance.
Remember, exercise should be implemented using the five phases of fitness that I discuss in our episode about exercise.
Sleep — Did you know that not getting enough sleep is a risk factor for developing diabetes?
Along with all the other problems that poor sleep hygiene can cause — irritability, depression, chronic fatigue, and heart disease, to name a few — you’re also at a higher risk of developing diabetes.
If you use wearable technology, track your sleep. Most people require at least seven hours of sleep per night. If you aren’t hitting that consistently, you need to focus on improving your sleep hygiene.
Make sure your room is dark, quiet, and cool. Don’t use screens for 30 minutes or more before bed and don’t eat any large meals for at least two hours before bedtime. If you have trouble falling asleep, try prayer or meditation to relax your mind and body.
3) I’m Diabetic and on Insulin — Should I Also Be on Metformin?
You may be asking this question if you’re curious whether you’re really attacking the root of diabetes, which is insulin resistance.
If diet and exercise aren’t enough, you may need medication. The drug of choice to treat insulin resistance is Metformin.
Metformin is a critical component of the diabetes medication regimen. If you are diabetic on insulin, you need to be on Metformin as well, unless you’ve got kidney disease.
Metformin works by increasing your body’s insulin sensitivity.
It is safe, and does not cause low blood sugar episodes. It may cause some GI upset in the first week or two of treatment, but that usually subsides.
It can be prescribed for anyone unless they have an allergy to it, or kidney disease.
I wouldn’t start with Metformin, but if diet and exercise are not yielding the outcomes that you want, adding medication may help.
If you’re on insulin, which your body is already ignoring, you’re giving your body way more than it needs. By simply adding Metformin, you will be able to reduce the amount of insulin that you’re exposing your body to, curbing the negative effects of that hyper-insulin state.
Listen, I hope you can see how passionate I am about this topic.
It’s a really big deal.
I hope you enjoyed this post on insulin resistance. If you don’t know if you’re insulin resistant, talk to your doctor about getting the recommended tests for it. And if you are insulin resistant, know that it can be reversed before it develops into diabetes.

Dr. Aaron Wenzel is a concierge physician specializing in the care of fast-moving entrepreneurs, executives, and public figures in the Nashville, TN area. Dr. Wenzel’s diverse life experience and extensive training in family medicine, emergency care, nutrition, and hormone replacement therapies give him the unique platform to provide unmatched care for his patients.





It’s really helpful article, I am a middle aged person and I like to google health related issues which I face. By the far this article is the best article i have read from the day i started googling. It’s detailed and knowledgeable.
Glad you enjoyed it, Ankur!