It’s time to talk about cholesterol, but not in the way you’re expecting.
Let’s start with the “facts” you’ve been taught to believe. Do these sound familiar?
Don’t eat foods that are high in cholesterol – they’ll kill you!
As long as your total cholesterol level is low, you’re safe.
Those high-fat foods will give you a heart attack.
After nearly 100 hours of deep research, I’ve uncovered a remarkable, devastating truth: our widely understood “facts” about cholesterol aren’t facts at all.
Which is exactly why I’m here with Jen Justus, my talented Nurse Practitioner and partner in crime, to help you understand the most important information about cholesterol that even your doctor may not know.
Though the biochemistry of cholesterol is complex, you don’t need to understand the technicalities in order to appreciate the bigger picture and take essential steps to improve your own health.
As always, Jen explains it best: “You can get really lost in all of the technicality and biochemistry of cholesterol, but what we’re intending to do today is to deliver it in a way that’s very easily understood and give you action steps: What do I need to do to make sure I’m taking every precaution I can to prevent this killer of humans?”
How to Understand Your Cholesterol Health
We all know that cholesterol plays a role in cardiovascular health and disease, but how, exactly? Even the professionals can’t always agree. Is it evil? Insignificant? Beneficial? There’s no one simple answer.
We have to understand cholesterol on a spectrum because its role in the body is so complex. Cholesterol is essential for life because it enables the body to build the structure of cell membranes, make hormones, and support metabolism. But cholesterol also plays a key role in the development of cardiovascular disease. As a result, cholesterol is highly debated, and most of the people who matter have it wrong.
“That’s a bold statement,” Jen reminds me. But I pride myself on taking the time to dig miles deep into topics that matter. Cardiovascular disease is one such topic that I’m continually trying to understand, and I can’t possibly do that without cracking the code on cholesterol.
To me, the scariest part was realizing that the data I uncovered wasn’t new. Some of it has been around for a decade, but it hasn’t been incorporated into medical texts yet. Critical pieces of science have unfolded over the last ten years, and most doctors are missing them!
Jen echoes my thoughts: “The standard medical community is behind when it comes to understanding and applying data to how we manage patients day to day – it’s concerning.”
When incidences of heart attack and stroke cause 1 in 4 deaths in America annually, and cholesterol plays a role in underlying cardiovascular disease, we have a critical responsibility to understand how the puzzle pieces fit together.
The Real Effects of Dietary Cholesterol
Cholesterol is a waxy, fat-like substance. Your body naturally makes all of the cholesterol it needs to perform essential functions like producing hormones and vitamin D. However, most of us still receive a secondary supply of cholesterol in our diets from animal sources. Eggs, meat, and dairy all contain dietary cholesterol.
When patients are diagnosed with high cholesterol, they’re told to eliminate dietary cholesterol immediately. These people suffer and panic for months, avoiding scrambled eggs and yogurt for fear of a heart attack. And when they return for their next round of testing, their cholesterol levels may still be sky-high.
That’s because, contrary to popular belief, dietary cholesterol has little to zero impact on your total cholesterol.
Fear of Fat: Should You Be Scared?
The debate over cholesterol quickly leads to another controversy: fat. I remember in the mid-1980s when fat became Public Enemy #1 virtually overnight. More than 30 years later, this myth still prevails.
Jen recalls that the low-fat fad influenced her family’s perception of food and health as well. “I grew up in a low-fat, high-carb household. I remember my mom saying, ‘You’re eating an avocado, do you know how many calories and fat are in that?’ and I would say, ‘But it’s good for me!’”
As Jen explains, there’s still a stigma around fat because people believe it automatically causes high cholesterol and obesity. Since the underlying thought process is logical, this false narrative has been able to survive so long. Yet it’s completely wrong.
The bottom line? Fat does not make you fat – excess blood sugar does. It’s not even debatable.
Parts of a Standard Lipid Panel
A cholesterol test is performed with a standard lipid panel. This blood test measures the amount of cholesterol in your blood using the following benchmarks:
- Total cholesterol
- High-density lipoprotein (HDL) cholesterol concentration
- Low-density lipoprotein (LDL) cholesterol concentration
- Triglycerides
This sounds simple and straight-forward, but in my research I’ve discovered that the information revealed in a lipid panel alone is not enough to confirm the presence or risk of cardiovascular disease.
The Real Meaning of HDL and LDL Cholesterol
Cholesterol molecules can only travel through the body when packaged inside of lipoproteins. This means that lipoproteins function as a shuttle to transport fatty substances throughout the extracellular water of your body and into cells and tissues.
Lipoproteins fall into many categories, but it’s the cholesterol-rich apolipoprotein B (apoB) that matters. About 98% of all apoB lipoproteins are low-density. In other words, they’re LDL cholesterol, the form that gets deposited into peripheral tissues and causes health problems. You can think of apoB as a cholesterol “delivery truck”.
Apolipoprotein A-1 (apoA-1) lipoproteins, on the other hand, support high-density (HDL) cholesterol. These “dump trucks” clean up and recycle cholesterol while nourishing cells and tissues with antioxidant and anti-inflammatory properties. The more HDL cholesterol you have naturally in your system, the better.
This is why it’s tempting to call LDL the “bad” cholesterol and HDL the “good” cholesterol, but these misnomers don’t paint the whole picture. While it’s helpful to know your LDL and HDL concentration numbers, they lack insight into the overall behavior of cholesterol within your body.
The Most Important Information You Need From a Lipid Panel
Despite overwhelming evidence from years of research, a standard lipid panel doesn’t provide the most critical information needed to predict cardiovascular risk. A lipid panel provides the concentration of LDL and HDL in the blood, but it’s not concentration that matters; it’s particle number.
In other words, the weight of LDL and HDL cholesterol particles doesn’t matter nearly as much as their quantity.
This explains why a vegan with a very low LDL concentration can appear healthy, then suddenly suffer a heart attack. If his doctor didn’t test his apoB particle numbers, nobody would have realized his risk of heart disease.
How Does This Relate to Atherosclerosis?
Arteries are blood vessels that feed oxygen-rich blood to tissue. Atherosclerosis develops when those arteries narrow and close off due to cholesterol-based plaque. This condition begins when apoB penetrates an artery’s protective lining and stays there. The presence of apoB in the endothelium triggers an immune response with inflammation and swelling, which creates even more space for apoB to accumulate. After enough time passes, this creates a cholesterol core of plaque in the arteries.
As plaque grows, it matures, calcifies, and hardens. The older plaque becomes, the more prone it is to rupture and travel into the bloodstream like a boulder in a river. Dislodged plaque blocks blood flow and eventually causes heart attack, stroke, tissue death, and other deadly complications.
This is so important to understand because the LDL concentration tested in a standard lipid panel is not reliably predictive of atherosclerosis. The apoB particles are the real culprit! More particles cause more damage.
When you only know your LDL concentration, you can only guess your risk of cardiovascular disease. When you’re armed with your apoB particle number, however, you can know your real risk.
Identifying Concordance and Discordance
When testing reveals a patient’s LDL concentration and apoB numbers are both similar or the same, concordance exists. On the other hand, when LDL concentration and apoB numbers not similar, discordance exists.
Discordance makes LDL concentration data unreliable, so it should signal a profound red flag to medical professionals. “This is very scary to me,” Jen admits. “The percentage of people who have a normal LDL concentration but a high apoB signaling red flags is one in four. It’s putting them at risk, and their doctor might miss it.”
Take, for example, the vegan with a low LDL concentration. At first glance, the vegan appears healthy. His LDL cholesterol levels are low, and he doesn’t eat any sources of dietary cholesterol that could potentially increase the amount of cholesterol in his blood. But if his doctor remains unaware of his dangerously high apoB particle numbers, the vegan’s true risk of cardiac disease won’t be revealed until he suffers a heart attack.
Concordance and discordance matter for everyone, not just vegans. Of all healthy adults who don’t smoke or have an underlying metabolic condition, 22% have discordance in their numbers. This means that one in four of all healthy adults are likely to believe they’re not at risk of cardiovascular disease because doctors will miss the red flags in their lipid panels.
The numbers are even worse for the remainder of adults, most of whom have diabetes, pre-diabetes, and undiagnosed diabetes. They have a rate of 63% discordance. Only with a complete understanding of cholesterol and testing can doctors and patients work together to identify discordance and act on it accordingly.
7 Simple Ways to Improve Your Cholesterol Health
I can’t overstate how important this topic is, but you don’t need to understand the technicalities to take action for your own health. By following these seven steps, you can improve your cholesterol health and optimize your wellness.
Step 1: Normalize Your Blood Sugar
“We can’t talk about this enough! It’s the holy grail,” Jen so accurately reminds us. You must normalize your blood sugar. Period. If you don’t take control of your blood sugar, you’ll develop diabetes, the gateway to nearly every Western disease, from obesity to Alzheimer’s.
Step 2: Know Your Numbers
Learning all of your numbers – blood pressure, cholesterol, blood sugar, triglycerides – is like ripping off a Band-Aid. You don’t know the condition of your body until you get to the other side. When it comes to cholesterol, give special attention to these numbers:
- LDL particle number (apoB)
- Hemoglobin A1C
- Ratio of triglycerides to HDL (TG:HDL)
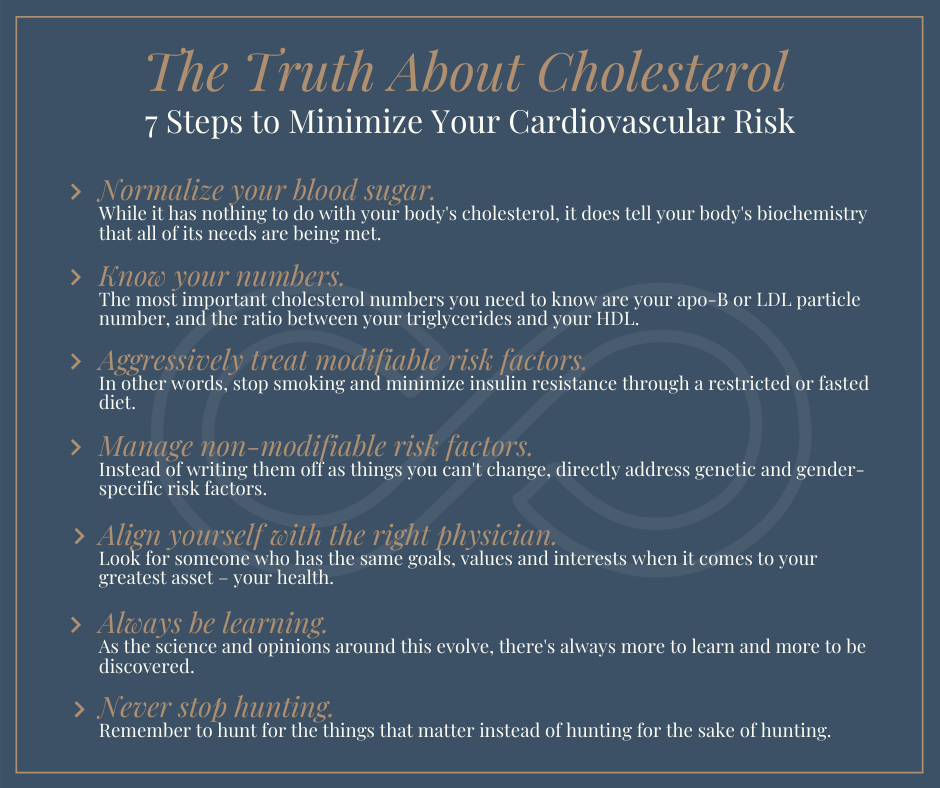 Step 3: Improve Modifiable Risk Factors
Step 3: Improve Modifiable Risk Factors
Modifiable risk factors threaten your heart health but are relatively easy to adjust. With proper lifestyle and dietary changes, you can reduce the impact of the following modifiable risk factors:
- Tobacco Use
- Alcohol consumption
- Lack of exercise
- High stress
- Inflammatory diet
Every additional risk factor makes it more difficult to escape the avalanche of cardiovascular disease, and every risk factor you eliminate makes it easier to improve your health.
Step 4: Manage Non-Modifiable Risk Factors
Certain heart disease risk factors can’t be changed or modified. They exist whether you like it or not, including:
- Age
- Gender
- Genetic profile
Since you can’t change these risk factors, it’s critical to manage them instead. Watch for warning signs and take actions that minimize your health risks and protect your body, such as preventative screenings.
Step 5: Find the Right Provider
Health is more than just the absence of disease – it’s the ability to thrive and live an active life. If your doctor isn’t committed to that shared goal, you may not be receiving the best care.
Your health is your most valuable asset, and you deserve a provider who will serve as a steward and trusted adviser. A real doctor-patient relationship cultivates compassion, trust, empathy, and communication.
Step 6: Never Stop Learning
Education is the most powerful tool at your disposal, and thanks to the internet it’s easier than ever to educate yourself. Find voices that you trust and continue to learn about the factors that influence your body, your life, and your happiness.
Step 7: Never Stop Hunting
Diseases don’t always stand in the open, wearing bright yellow and shouting your name. You have to hunt for them, find them, and control them before they have the chance to control you.
This is why I couldn’t possibly say this with more conviction:
Go to your doctor and tell them, “I need to know my apoB and/or LDL particle numbers.”
Without those numbers, you don’t really know your risk of heart disease at all.
Don’t let the technicalities of cholesterol scare you. If you want to understand it, you can, but at the end of the day, the most powerful way to protect your body is to take action.

Dr. Aaron Wenzel is a concierge physician specializing in the care of fast-moving entrepreneurs, executives, and public figures in the Nashville, TN area. Dr. Wenzel’s diverse life experience and extensive training in family medicine, emergency care, nutrition, and hormone replacement therapies give him the unique platform to provide unmatched care for his patients.






