If you’ve found yourself sneezing through spring or wondering whether certain foods are causing mysterious symptoms, you’re not alone. Allergies affect millions of Americans, yet many people struggle to understand what’s triggering their symptoms or how to find real relief.
I recently sat down with my colleague Dr. Jennifer Ker, a board-certified allergist-immunologist with Heritage Medical Associates in Nashville, to discuss some of the most common questions members bring to me about allergies.
Dr. Ker brings impressive credentials to this conversation, earning her medical degree from the Medical College of Ohio and completing both her pediatrics residency and allergy and immunology fellowship at Vanderbilt University. She also holds a Master of Science in Neurobiology and Physiology from Northwestern University and is a fellow of both the American College of Allergy, Asthma, and Immunology and the American Academy of Allergy, Asthma, and Immunology.
That combination of intellectual challenge and immediate patient impact drew Dr. Ker to allergy care, and I was eager to get her insights into a topic I felt less equipped to address.
When Spring Becomes a Struggle: Environmental Allergies
The spring pollen season is the dread of many of my members, bringing a predictable wave of distressing symptoms. But Dr. Ker reminds us that not everyone’s allergies follow the same pattern.
The classic spring allergy symptoms include eye drainage and itching, sometimes even eye swelling. Nasal congestion, drainage, and mucus in the throat are common complaints. For some patients, particularly those with asthma, the breathing challenges can become more serious — moving beyond a mild cough to actual wheezing and significant trouble breathing.
The tree pollens typically arrive mid-February through April and May, though Dr. Ker notes they came later this year. Grass pollens follow in April, May, and June. But here’s where things get interesting: Many people assume they know what they’re allergic to based on when their symptoms appear, only to discover the real culprit is something entirely different.
The Value of Knowing Your Triggers
When patients tell Dr. Ker, “It’s the spring, it’s the spring every year,” she often digs deeper. Through testing, she might discover they’re actually allergic to outdoor molds or dust mites, with only a mild grass allergy contributing to their symptoms.
Why does this matter? Understanding your specific allergens isn’t just to satisfy your curiosity — it gives you more opportunity to control your exposure and improve your quality of life.
Testing comes in two forms: blood tests and skin tests. Skin testing remains the gold standard in medicine and is considered the most accurate way to evaluate allergies. Both methods can test for a broad variety of allergens, including trees, grasses, weeds, indoor and outdoor molds, dust mites, and pet dander. Both can also test for various food allergens, though blood testing may offer a slightly broader panel for less common foods and spices.
These tests complement each other, helping allergists get the full picture on a patient’s allergies. Dr. Ker explains that if a patient seems to struggle with spring pollen but the skin test doesn’t provide answers, she might send blood work to investigate further (and vice versa). Or, a patient may have a negative blood test for peanuts but a strongly positive skin test.
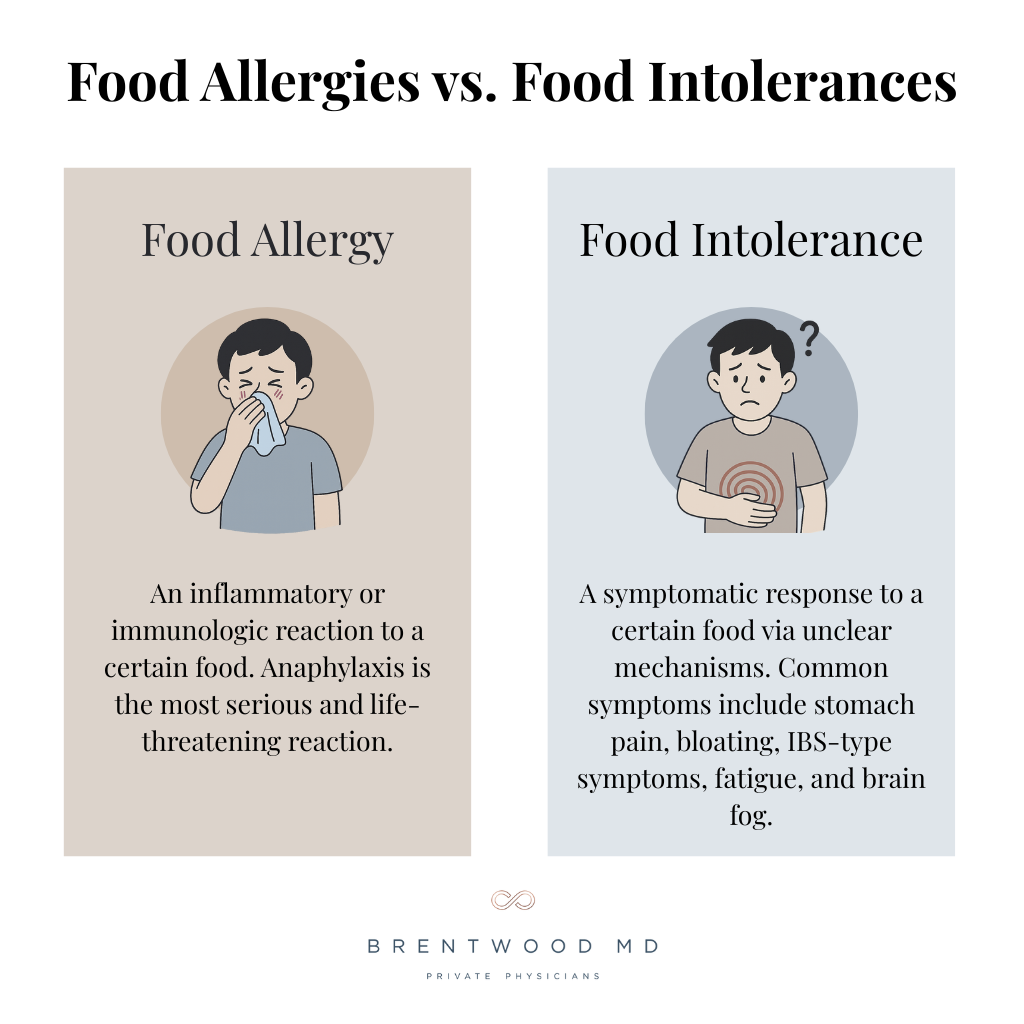
Food Allergies vs. Food Intolerances: Understanding the Difference
One area where I see tremendous confusion — and where Dr. Ker’s expertise proves invaluable — is distinguishing between food allergies and food intolerances.
A food allergy, in its general definition, is simply an inflammatory or immunologic reaction to a food. This broad definition could technically encompass food intolerances, but we traditionally use “allergy” to describe the more serious, IgE-mediated reactions that carry a risk of anaphylaxis. These involve foods entering the body and creating an allergic cascade resulting in hives, swelling, trouble breathing, and even passing out from low blood pressure. The usual suspects here include peanuts, tree nuts, shellfish, and sometimes fish. In younger children, milk and eggs may also commonly trigger these reactions.
Food intolerances present a different challenge. Dr. Ker admits that medicine still has significant gaps in understanding what inflammatory cascade occurs with food intolerances. The symptoms can be quite debilitating — stomach pain, bloating, IBS-type symptoms, fatigue, and brain fog — but we don’t yet have a perfect diagnostic test for them.
What we do know? When patients discover foods that trigger these symptoms and eliminate them, they feel better. Patients also stick with their elimination diets at remarkably high rates, unlike typical weight loss diets, where compliance hovers near zero. “That tells me there’s something really going on there,” Dr. Ker says.
Start With Fiber: The Gut Microbiome Connection
When I asked Dr. Ker where to start with patients experiencing food intolerance symptoms, her answer surprised me: fiber.
The diversity of microbes in our gut depends heavily on fiber. But the typical American diet includes only about 10 grams of fiber daily, when 25 to 30 grams is ideal. Those gut microbes communicate with our immune system and nervous system, and how they eat matters. Their best food? Fiber.
Before eliminating foods, Dr. Ker recommends starting with a healthy, high-fiber, plant-forward diet — like the Mediterranean diet. “It’s not all Greek salads and chicken kebabs,” she clarifies. “It’s actually a lot of legumes. It’s a lot of beans.” After a month of 25 to 30 grams of fiber daily, patients may notice improvement in their gut symptoms.
If symptoms persist, however, she moves to elimination trials, typically starting with wheat and dairy — the two most common food intolerances. The key is omitting a food for at least two weeks, then putting it back in to assess how you feel. This prevents the placebo effect from leading you astray and helps you genuinely understand your body’s response.
Beyond fiber, the only supplement with solid data supporting reduced allergic inflammation is omega fatty acids. “Other things that can increase the diversity of your gut microbiome are getting a good night’s sleep and exercise,” Dr. Ker says. “So I oftentimes will mention those because they work.”
Navigating Food Allergies in Children
For parents dealing with a child’s severe nut allergy, the challenges can feel overwhelming. Dr. Ker acknowledges the stress and the difficulty: “I think it’s important to just agree that it’s tough,” she says. “It’s very difficult to avoid a food allergen strictly.”
Fortunately, most children with food allergies — even nut allergies — aren’t so sensitive that they have to avoid every part per billion possible. But accidental exposures to larger amounts can and do happen.
Dr. Ker shares that in her experience, though, kids often become remarkably capable self-advocates. She’s seen four-year-olds double-check their parents when handed crackers, asking, “Mom, does that have nuts in it?” The key is teaching children that by simply not putting a food in their mouth, they stay safe — even if they’re sitting next to someone eating nuts at the lunch table.
Research shows no positive difference in accident rates between nut-free tables and regular tables. National allergy societies now encourage self-advocacy rather than isolation. Children can learn what they can and cannot eat, which also serves to reduce anxiety and build confidence.
For cases in which accidental exposure does occur, there’s also promising news: A medication now exists that significantly improves safety from accidental exposures — a life-changing development for families with severe food allergies.
Managing Environmental Allergies: Finding What Works
With two full aisles of allergy medications at any pharmacy, how do you choose? Dr. Ker breaks down the basics:
- Antihistamines (Zyrtec, Allegra, Claritin) work well for itching, dripping, and sneezing and are less sedating than Benadryl.
- Nasal steroid sprays (Flonase, Nasacort) reduce inflammation in the back of the nose and sinuses, helping with congestion.
- Nasal antihistamine sprays (Astepro) combine the benefits of both approaches.
Patients respond differently to these medications, so Dr. Ker tends to suggest patients choose whichever medication works best for them. So if Zyrtec makes you tired, try Allegra. If antihistamine sprays offer relief, opt for those.
She also recommends giving any new antihistamine no more than two days to assess its effectiveness. You’ll know pretty quickly if it’s helping.
When to Consider Allergy Shots
Dr. Ker reserves immunotherapy — allergy shots or drops — primarily for patients whose environmental allergies affect their airways, creating asthma symptoms with any regularity. If allergies impact your sleep or contribute to sleep apnea, that’s another indication to consider this next level of care.
While allergy drops exist, Dr. Ker prefers shots simply because they tend to work better. “If we’re going to go for this process, we’re going to go for the one that’s going to be the most effective.”
Allergy shots can significantly reduce airway inflammation, decrease asthma symptoms, allow less medication use, and even help the immune system fight viral infections better by removing allergic inflammation.
In children with severe environmental allergies, a course of allergy shots can actually forestall asthma development — a powerful preventive measure.
Allergy shots are not appropriate for food allergies, according to Dr. Ker, as they present significant risks.
Asthma: More Options Than Ever
Asthma management has evolved dramatically over recent years. Dr. Ker emphasizes that asthma is simply a pattern of coughing and wheezing, but understanding what drives that pattern helps us choose the right treatment.
For intermittent asthma triggered only by exercise or cold air, simple rescue inhalers used 20 minutes before activity may suffice. For persistent asthma, identifying triggers becomes crucial. Is it allergies (indoor or outdoor)? Acid reflux? Nasal polyps? Each driver suggests different treatment approaches.
Treatment can range from stronger inhalers to biologics, which are medications that target specific parts of the immune system to strategically calm inflammation. For allergic asthma, Dr. Ker typically recommends allergy injections before biologics, given immunotherapy’s century-long track record and potential to truly modify the immune system rather than requiring chronic medication.
Finding the Right Care
Allergies don’t have to control your life, whether you’re dealing with spring pollen, food sensitivities, or asthma. The key is accurate diagnosis, appropriate treatment, and expert guidance to navigate the complexities.
If you’re struggling with allergy symptoms that impact your quality of life, consider consulting with a specialist like Dr. Ker at one of Heritage Medical Associates’ offices in the Nashville area.
At Brentwood MD, we value building a strong network of specialists we trust. Dr. Ker has been invaluable to many of my patients, helping them finally understand what’s triggering their symptoms and finding effective solutions. You deserve to breathe easy. So if allergies are troubling you, don’t hesitate to bring them up in your next appointment!

Dr. Wright joined Brentwood MD in 2022 as the model allows him to spend more time connecting with patients and build a foundation of exceptional care. He is a Nashville native and completed his family medicine residency at the University of Tennessee Health Science Center, where he also served as Chief Resident. He believes that your health deserves a prominent position on your priority list, and would be honored to serve you and your family.