Download file | Play in new window | |
Recently on the podcast, Jen Justus and I talked about perhaps one of the most frightening health-related topics on the planet: cancer.
Cancer is the number two killer of human beings, second only to heart disease. In fact, approximately every minute someone in the United States dies from cancer.
Cancer is one of the most concerning conditions for anyone who wants to live a long, healthy life. Although cancer has been around for a long time, we still don’t detect many cancers until they’re advanced. Screening recommendations are complicated, confusing, and vary by organization. Testing and treatment can be expensive.
So today we want to talk about where we are with cancer screening tests, the old versus the new approach, and some amazing new technology to consider in your cancer screening strategy.
What Is Cancer Screening?
Early detection is the key to beating cancer. If you can catch it before it becomes advanced or widespread, you have a much better starting place from which to fight and win.
Cancer screening tests are the only method we have to detect cancer early. Evaluating symptoms doesn’t cut it. By the time you notice symptoms, early detection is no longer possible.
We have different cancer screening tests for different types of cancer. We use mammograms to detect breast cancer in women, blood tests and imaging to detect prostate cancer in men, and colonoscopies to detect colon cancer in everyone. Imaging, blood tests, and special exams are the best tools we have right now for cancer detection.
The scary thing is, most cancers — even some of the most deadly — have no standard screening tests for early detection.
Where Do Cancer Screening Recommendations Come From?
Government bodies and organizations use a method called population health to produce recommendations for cancer screening tests. In other words, they look at the entire population and ask questions like:
- At what age did a certain cancer become evident in most people?
- Would screening have caught it?
- What test would reliably catch it early in the largest percentage of people?
- How frequently is that test needed to catch the cancer in most people?
They then create early detection guidelines for the population as a whole.
But population health doesn’t consider the individual. People with certain risk factors, like a family history of cancer, fall outside the perspective of population health. They’re at higher risk, and they need cancer screening tests earlier than others. Following guidelines created for the general population could cost them the chance to detect cancer early.
The Old Way of Screening for Cancer
Conflicting Standards and Recommendations
Should women start getting mammograms at age 40 or 50? Should they get them every year, or every two or three years? Should men get tested for prostate cancer at 40, 45, or never unless they have a high risk factor?
One reason early detection is so difficult is that the standards for screening are confusing and conflicting. High-level, reputable organizations like the American Cancer Society, the Centers for Disease Control, and the United States Preventative Services Task Force all have different standards for cancer screening. Recommendations vary by country as well.
Many recommendations for cancer screening tests put the onus on the patient to request testing from their doctor. This isn’t necessarily an issue, but it can mean insurance won’t cover the test based on their standards of screening. This can keep patients from getting the early detection tests they need.
Don’t Skip Standard Screenings
While guidelines for recommended cancer screening tests can be confusing, don’t let that keep you from getting them. These basic cancer screening tests could save your life:
- Mammograms and Pap smears for women
- Prostate cancer screening for men
- Colonoscopy for men and women over age 45
Talk with your doctor about your risk factors, health, and family history to decide when you should get which of the standard tests, and how often.
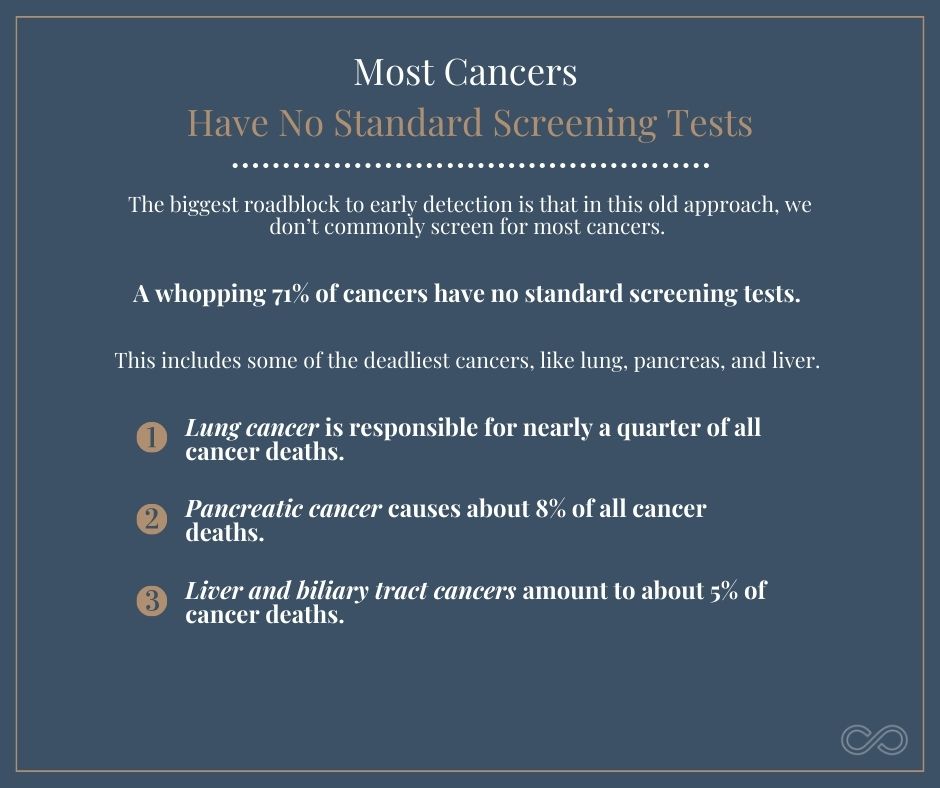
Most Cancers Have No Standard Screening Tests
The biggest roadblock to early detection is that in this old approach, we don’t commonly screen for most cancers.
A whopping 71% of cancers have no standard screening tests.
This includes some of the deadliest cancers, like lung, pancreas, and liver.
- Lung cancer is responsible for nearly a quarter of all cancer deaths. (And it’s not only smokers who are at risk.)
- Pancreatic cancer causes about 8% of all cancer deaths — similar to the percentage of breast cancer deaths — yet we screen for breast cancer, and not pancreatic cancer.
- Liver and biliary tract cancers amount to about 5% of cancer deaths and have no standard screening.
Most of the time, we only check for these other cancers in response to symptoms. You feel tenderness or a lump, you experience shortness of breath or unusual tiredness, or you have some other physical sign that something isn’t right. By then, the cancer has often already progressed.
When we take this approach, treatment becomes reactive rather than proactive. We take a defensive stance, which limits our options and reduces the patient’s chance of survival.
We have to do better.
The New Way of Screening for Cancer
The new way of approaching cancer screening involves going on the offense. We want to actively hunt for the top dangers that could take us off the planet, not sit back and wait for them to surprise us.
And an exciting new technology has given us a new way to hunt. It’s called the Galleri test by GRAIL.
The Galleri test can detect more than 50 different types of cancers, and all it requires is a simple blood draw. No invasive testing, no radiation exposure, no danger.
All the cells in our body, including cancer cells, secrete DNA into our bloodstream. The Galleri test examines the DNA present in your blood and screens it for abnormal (cancerous) DNA particles. You might think of it as a blood biopsy.
The method allows the Galleri test to identify cancer extremely early — long before symptoms show up.
In addition to detecting signals of cancer with a high level of accuracy, the Galleri test can also determine the origin of those signals. This can save valuable time, giving doctors an immediate idea of the location of the cancer and letting them zero in to begin treatment as quickly as possible.
Benefits of the Galleri Test
The Galleri blood test is one of the most proactive moves you can make against cancer. You aren’t just reacting to the signs and symptoms that come with advanced-stage disease; you’re actively looking and preventing it from ever getting that far.
The cost of the Galleri test is relatively affordable compared to many other cancer screening tests, especially for the peace of mind it can provide. Depending on the health care provider, the Galleri test costs around $1,000. It takes about ten days to get the results.
This test is designed to be specific and sensitive, meaning it can detect even small amounts of abnormal particles. Since cancer doesn’t develop overnight, catching these abnormal particles early saves a lot of valuable time.
One of the nice things about the Galleri test compared to some other cancer screening tests is how simple it is. All it requires is a simple blood draw, and you don’t even have to fast.
Limitations of the Galleri Test
While the Galleri test is an amazing tool for our arsenal in the fight against cancer, it isn’t a silver bullet. Like any test, it’s not perfect, and it should NOT replace other standard cancer screening tests like mammograms, Pap smears, prostate screening, and colonoscopies.
One drawback is that the $1,000 price tag might be beyond some people’s budget. Unfortunately, insurance companies don’t yet cover the Galleri test, and there’s no sign of them doing so in the near future.
Another limitation of the Galleri test is the risk of a false positive. The risk is low — about 1 in 200, or 0.5% — but it’s there. A false positive can occur simply because the test is wrong, or because the test detects a tumor so small that other diagnostic tools can’t find it.
A false positive can cause serious distress and suffering, so it’s important to be aware of this risk ahead of time. However, if you do receive a false positive, GRAIL will pay for subsequent repeat testing at no cost to you.
Another limitation of the Galleri test is that because it’s so new, we don’t have a standard recommendation on how often to do it. Health care providers who offer this test do so on a case-by-case basis. This will depend on you, your health and family history, your risk profile, and your desire and ability to cover the cost of the test.
The Bottom Line
As the number two killer of humans, cancer is a real threat to our health. We don’t have recommended cancer screening tests for most of the cancers that plague us, so we need to move beyond what’s recommended and take an offensive approach.
No one should skip the standard recommended cancer screening tests, but that’s just the bare minimum of what we can do against this menace. Each of us also needs to find a health care team who will support an offensive approach to early cancer detection. This may mean starting standard screenings earlier than recommended based on your history, or it may mean discussing the Galleri test with your doctor.
Some cancer testing may not be covered by insurance, whether it’s an early mammogram or a Galleri test. But if you have a strong family history of cancer or another major risk factor, finding a way to get these crucial tests could save your life.

Dr. Aaron Wenzel is a concierge physician specializing in the care of fast-moving entrepreneurs, executives, and public figures in the Nashville, TN area. Dr. Wenzel’s diverse life experience and extensive training in family medicine, emergency care, nutrition, and hormone replacement therapies give him the unique platform to provide unmatched care for his patients.