Download file | Play in new window | |
Heart disease is the number one killer of humans. In fact, every 36 seconds, someone in the United States dies from cardiovascular disease.
And this isn’t just a problem in the U.S.; it’s worldwide.
Unless we have simultaneous breakthroughs in human behavior, society, and science, it will continue to be the number one killer of humans worldwide.
We talk a lot about heart disease, so we know our patients and our audience aren’t strangers to this topic. What we want to do today is offer some tactical help for knowing and addressing your risk.
What Is Heart Disease?
At the highest level, atherosclerosis — the hardening of arterial walls — causes heart disease.
All tissue needs oxygen; oxygen comes through blood; oxygenated blood travels through arteries. As atherosclerosis occurs, plaques form inside the arteries, narrowing those passageways and minimizing blood flow.
But the really scary things are unstable soft plaques that break off in fragments, travel downstream, and become lodged in smaller arterioles, blocking blood flow and causing tissue death.
If this happens in the heart, we call it a heart attack. If it happens in the brain, we call it a stroke.
Looking at Heart Disease the Old Way
In the old way of looking at heart disease, you either have it or you don’t.
The problem with this view is that all disease exists on a spectrum with health at one end and active disease at the other. But there’s a whole range of possibilities in between those two, and we shouldn’t wait until you reach the disease end of the spectrum to start addressing health issues.
By only asking, “Do you have this disease,” we miss out on any opportunity to address (and prevent) disease before it arrives. We take a defensive posture that reacts to obvious symptoms once they arise.
But the problem is that once symptoms arise, you already have advanced disease.
The old approach is the reason why, after all these years, all our experience, and all medicine’s scientific breakthroughs, we still aren’t any closer to preventing heart disease than we were decades ago. It’s still our number one killer, and we’re still on the defense.
Looking at Heart Disease the New Way
The good news is that there’s a new way of looking at heart disease.
Jen and I, and a whole group of other like-minded healthcare professionals, observed that with the old way, people just kept getting sicker and sicker. In fact, health care wasn’t really “health” care at all; it was sick care. Our industry had become simply the management of disease and the desperate attempt to keep patients from dying.
And it wasn’t working.
Because of medicine’s old defensive approach, cardiovascular disease has continued to climb. In fact, the American Heart Association projects that by 2035, more than 130 million people in the U.S. will have cardiovascular disease.
So we went on the offense.
Patients don’t just wake up one day and suddenly have heart disease. It’s a slow burn, and it happens over years and decades.
So instead of asking, “Do you have heart disease,” we ask, “Where on the disease spectrum do you fall?” We perform tests and screenings that look for more specific precursors to heart disease, not just for the alarm bells that mean heart disease has arrived.
We get a picture of where people are on the disease spectrum, and we can address contributing factors well before they result in full-blown disease.
Old Tests vs. New Tests
If you see a doctor regularly, they probably check your weight, total cholesterol, and blood pressure, and look at your family history.
If you’re a little overweight, your doctor might tell you to eat less and exercise more. If your blood pressure or cholesterol is a little high, they might put you on medication.
If you’re lucky, you might get a baseline EKG or a stress test.
But this tells you very little about your risk for future heart disease and where you fall on the disease spectrum.
With the new approach, you and your doctor become hunters; you hunt for the health issues that could take you off the planet. And that means looking for root causes.
One of the main root causes of heart disease is metabolic disease.
Like heart disease, metabolic disease slowly builds up as the body becomes insulin resistant. From here, high blood sugar damages the blood vessels and nerves and causes elevated insulin levels, dangerous lipid profiles, and high blood pressure, which all lead to heart disease.
Knowing these metabolic markers means we can test for them.
So on our hunt for heart disease, we look for metabolic disease factors like insulin resistance, inflammation, triglyceride-to-HDL ratio, fatty liver, carbohydrate processing, and more. And if we identify issues in these areas, we can address them — much more easily and effectively than we could address advanced heart disease.
We also use a special diagnostic device to test for visceral fat. This is fat deep in your body, surrounding your organs. It’s very pro-inflammatory and puts you at huge risk for heart disease. If we discover visceral fat, we can work aggressively to eliminate it at all costs.
We look at your family history. Did either of your parents have an early heart attack? Do they have high cholesterol or blood pressure? When did it start?
And we closely consider your lifestyle. Are you under consistent stress? Do you get enough good quality sleep? We can track these factors using wearable technology to provide great insights into your risk factors and how you can modify them.
Sick Care vs. Health Care
To be fair, our concierge model of practice gives us more flexibility and freedom to order the more detailed tests mentioned above and to spend more time with each patient, since we aren’t bound by any insurance constraints.
This goes to the root of why the old way of approaching heart disease has failed. The dominant model of healthcare, which is insurance-based, doesn’t focus on prevention.
It’s not designed to keep you healthy by preventing illness. It’s designed to keep you from dying, even if that means you stay sick.
So unless your sickness is bad enough to require a new medication, treatment, or procedure, you’re just being managed.
However, even if you’re stuck working within the constraints of insurance, there is hope. Make a note of the tests mentioned in this post and ask your doctor to order them. They may be able to bill for them in a way that insurance covers. Or, since many of these tests are fairly inexpensive, you could opt to pay cash.
Even if a test is a couple of hundred dollars out of pocket, isn’t that worth preventing a heart attack five years down the road?
You may run into a physician who’s reluctant to order some or all of these tests. They may be unfamiliar with the tests, or they may not know what to do with the results. Or, they may be reluctant because of insurance constraints.
Whatever the reason, it’s important to find a physician and healthcare team who are committed to helping you hunt for and mitigate your risk factors. And you might have to make some changes to find that team.
With the right team, even in an insurance-based practice, you can increase your chances of managing heart disease before it becomes a serious problem. You just have to know what to ask for.
Take Action
Once you identify and quantify your risk factors, you’ll have enormous insight into where you lie on the disease spectrum.
And once you know, you can make significant strides toward lowering your risk of developing heart disease.
Modifiable vs. Non-Modifiable
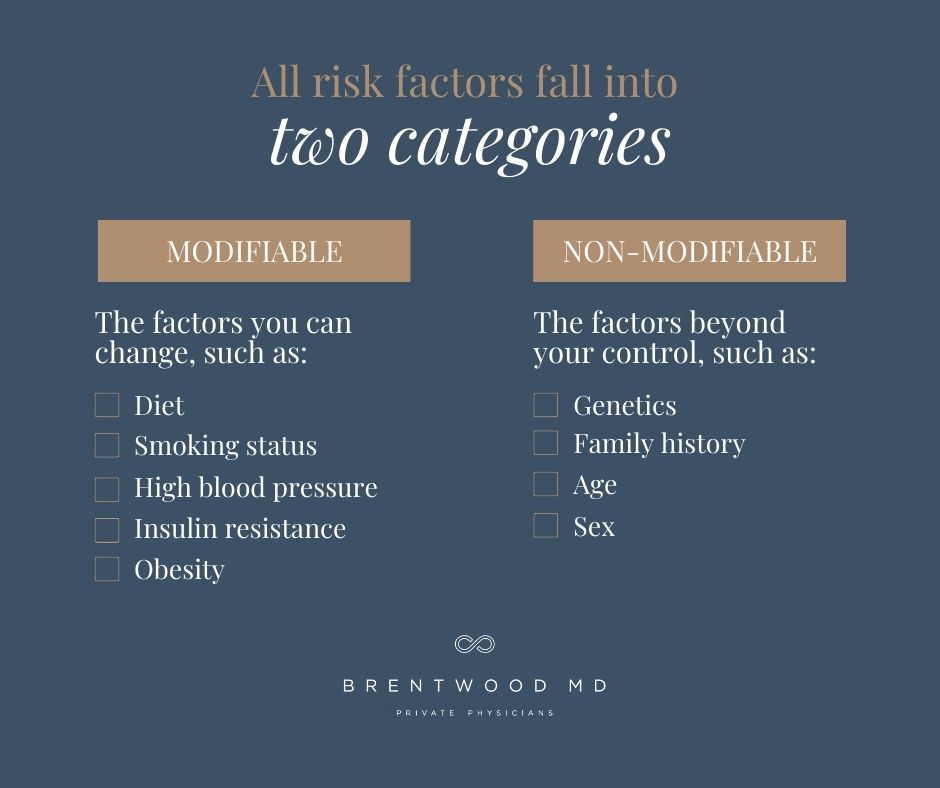
All risk factors fall into two categories: modifiable and non-modifiable.
Modifiable risk factors are the factors you can change, such as diet, smoking status, high blood pressure, insulin resistance, and obesity. Under the old approach, you wouldn’t try to modify until disease showed up. Even if you received a borderline diagnosis, this had been normalized to the point of just managing the condition instead of putting in the effort to reverse it.
But under the new approach, we realize there’s no such thing as borderline. There’s only early disease. And addressing our modifiable risk factors can reverse it.
Non-modifiable risk factors are factors beyond your control, like genetics, family history, age, and sex. There’s really nothing you can do about those things, but you can keep your eyes on them and manage them.
Age, for example, will always be a risk factor for heart disease. And you can’t change your age. What you can do, however, is focus on the early accelerators of heart disease — the modifiable risk factors that will cause you to develop heart disease at 50 rather than 90.
Tests: Good, Better, Best
At minimum, you’ll want to make sure you get at least the most basic blood work done. This includes a CBC, a CMP, a hemoglobin A1C, and a basic fasting lipid panel. These are the tests you’d usually get under the old approach to heart disease, but they’re better than nothing.
To move up to the next level of prevention, the most important thing you can do is to get an idea of where you are on the insulin sensitivity spectrum. You can find this through a combination of wearable technology and annual blood work.
Then, in addition to the basic blood tests, I recommend adding your LDL particle number (or APO B), Lp(a) (lipoprotein a), fasting insulin, APOE genotype, and possibly some glucose tolerance testing.
In the new way of approaching heart disease, we have some incredibly advanced new tests that are far more accurate and far more meaningful than the old screening tools like an EKG.
A cardiac CT calcium score, for example, could save your life. This test takes a noninvasive look at the calcified plaque in your arteries and gives us an excellent idea of your risk for heart attack or stroke.
Everyone over 50 should be getting a baseline calcium score, as well as everyone in their 40s with a heightened risk factor. Continued testing every few years based on risk is an easy way to keep track of where you are on the disease spectrum.
There are also some incredible tests available that show how well the blood is flowing through your heart vessels and whether there are any blockages to worry about. And it’s all virtual, without the invasiveness and risk of an actual heart cath.
We’ve used one test called HeartFlow and found it very useful. Now, we have an even newer technology called Cleerly, which works similarly but also shows us whether plaque is hard or soft plaque. This is important because, as we mentioned above, soft plaque is more unstable and dangerous.
All of this testing is meant to change the dynamic of our approach to heart disease. Instead of waiting until irreversible disease sets in and invasive procedures like stent placement and bypass surgery become necessary, we want to stop heart disease before it starts.
The Bottom Line
By the time a human being is 90, they will have atherosclerosis. But they may not have heart disease.
If you want to delay — and possibly even prevent — heart disease, look for a tailored approach to your healthcare. Find a doctor and a team who are willing to adopt a new way of approaching heart disease.
This is the only life you get, so make sure it’s the healthiest, longest, happiest life possible.

Dr. Aaron Wenzel is a concierge physician specializing in the care of fast-moving entrepreneurs, executives, and public figures in the Nashville, TN area. Dr. Wenzel’s diverse life experience and extensive training in family medicine, emergency care, nutrition, and hormone replacement therapies give him the unique platform to provide unmatched care for his patients.