Download file | Play in new window | Duration: 00:29:37 | Recorded on May 19, 2022
This month on the podcast, Jen and I talk all about enemy #1: metabolic disease.
If we want to improve the health and well-being of our society, metabolic disease is the single area in which we have to do a better job.
We’ve talked about metabolic disease before in our post on metabolic syndrome. But this topic is so important — and we reference it so much — that I think it’s time for a deeper dive.
Today we’ll talk about what metabolic disease is, why it happens, and five actionable ways to delay its onset.
Metabolic Disease Is a Disease of Abundance
Simply put, metabolic disease is energy dysmanagement. It exists (and we tend to map toward it) because we live in an age of perpetual abundance.
In countries suffering scarcity, you don’t have people developing the metabolic diseases that run rampant here. Instead, you have people dying of hunger, infectious diseases, war, and more. But not diabetes.
Nobody gets off the hook. There’s a tradeoff, whether you’re in a state of abundance or scarcity; the vulnerabilities are just different.
In the United States, where food is plentiful, metabolic disease is our vulnerability. Does that mean everyone always has enough to eat? Sadly, it doesn’t.
But consider the cultural changes that have taken place alongside the explosion of metabolic diseases in this country.
Abundant Access to Food
In years past, dining at a restaurant was a treat, and restaurants were much fewer and farther between. People mostly cooked and ate at home.
Fast food didn’t gain a firm foothold until the ’50s, and casual family dining took ground in the ’60s. Over the next few decades, restaurant chains proliferated and frequent eating out became the norm. At the same time, 20th and 21st century jobs often kept people in sedentary positions most of the day.
During these decades, incidence of metabolic diseases like diabetes skyrocketed.
Today, with the advent of food-delivery apps like GrubHub and Uber Eats, people have easier access to food — with less expenditure of effort — than ever.
Abundant Intake of Energy
With all this easy access to calorie-dense foods, we’ve been taking in more energy than we expend for decades. And our metabolisms are not happy with us.
Our metabolism is the set of mechanisms by which we use food to create energy. But when we overload it with energy we never use, this energy dysmanagement results in metabolic inefficiencies. When metabolisms become inefficient, we see metabolic diseases emerge.
Our bodies are designed to keep us alive during scarcity by storing fat in our cells during times of abundance and pulling fat from our cells during times of famine. The problem today is, for most of us, the famine never comes.
Instead, we’re constantly pushing more energy into our fat cells without ever recreating an environment where we need to take it back out again.
We’re constantly in an overfed state, often with very poor-quality foods.
Less Math, More Science
Despite conventional wisdom on weight loss, the obesity epidemic isn’t a math problem. It’s a biochemistry problem.
Calories do matter, but not all calories are created equal. If you’ve ever tried to “diet” by counting calories and couldn’t lose weight or keep it off, it’s not because you’re just bad at dieting. It’s because you need an approach that addresses weight loss from a hormonal perspective.
For example, highly processed, highly refined carbohydrates trigger massive surges in blood sugar, insulin response, and insulin resistance, which is the gateway for metabolic disease. So even when you keep to fewer calories, if most of them come from this type of food, you won’t lose much weight. And you certainly won’t fight off metabolic disease.
Ultimately, an abundance of calories, especially in the form of these poor-quality foods, is just too much for our bodies: too much blood pressure, too much blood sugar, too much cell division, too much everything. And it fuels the flames of cancer, obesity, heart disease, cognitive decline, and so many other problems.
Delay vs. Prevent
Metabolic disease is a condition of living in a world of abundance. It’s a disease of humanity, and if you’re around long enough, it will crop up in some form eventually.
But just because we can’t prevent it doesn’t mean we can’t delay it.
Often at first, metabolic diseases don’t cause major problems if they’re well controlled. But after 20 years with, say, diabetes, you may experience kidney issues, vision loss, and other side effects.
So would you rather have diabetes at 37? Or 57? What about 87? If you develop diabetes in your 80s (and keep it well controlled), those side effects won’t plague you until 100. But if you’re middle-aged? You’ll have to deal with those side effects much earlier in life.
This is what makes delaying the onset of metabolic disease so important. And if you can delay it long enough, you may even prevent it altogether.
How To Delay Metabolic Disease for Two Camps
Metabolic disease doesn’t happen all at once. It accumulates over a lifetime of decisions. And it really isn’t anyone’s fault. Most of human history was a history of scarcity. Our bodies simply don’t know how to operate with all this abundance.
So while the curve will always trend toward metabolic disease, your decisions influence how quickly that curve accelerates.
The only way to actually prevent metabolic disease is to delay it as long as possible. To do this, you must have a strategy.
In our experience, people fall into one of two camps. Let’s look at both, and at the appropriate delaying strategy for each.
1st Camp: You Know You’re Not Healthy
The people in the first camp are on the accelerated curve. They see warning signs like borderline hypertension, high cholesterol, and extra weight.
This can seem discouraging, but in reality, it’s an opportunity. It’s an opportunity to go from defense to offense, to take control and hit metabolic disease hard.
The result of offense is delay. And the sooner you get started, the better you’ll be able to delay or even prevent some of the more worrisome outcomes.
There is still an opportunity to slow that curve. The key is to take action immediately.
2nd Camp: You’re In Pristine Metabolic Condition
This is the camp of people who are healthy and have no warning signs of metabolic disease. They eat right, are active, and have healthy blood tests and stats.
But they’re still on that curve. It’s a slower curve than the first camp, but they’re on it.
Here’s the twist: Healthy people need to be on the offense, too.
Because metabolic disease is the default destination, complacency will always end up there. This is a forever game; you have to care forever.
So, just like the first camp, people in pristine metabolic condition must also take immediate, offensive action to delay metabolic disease as long as possible.
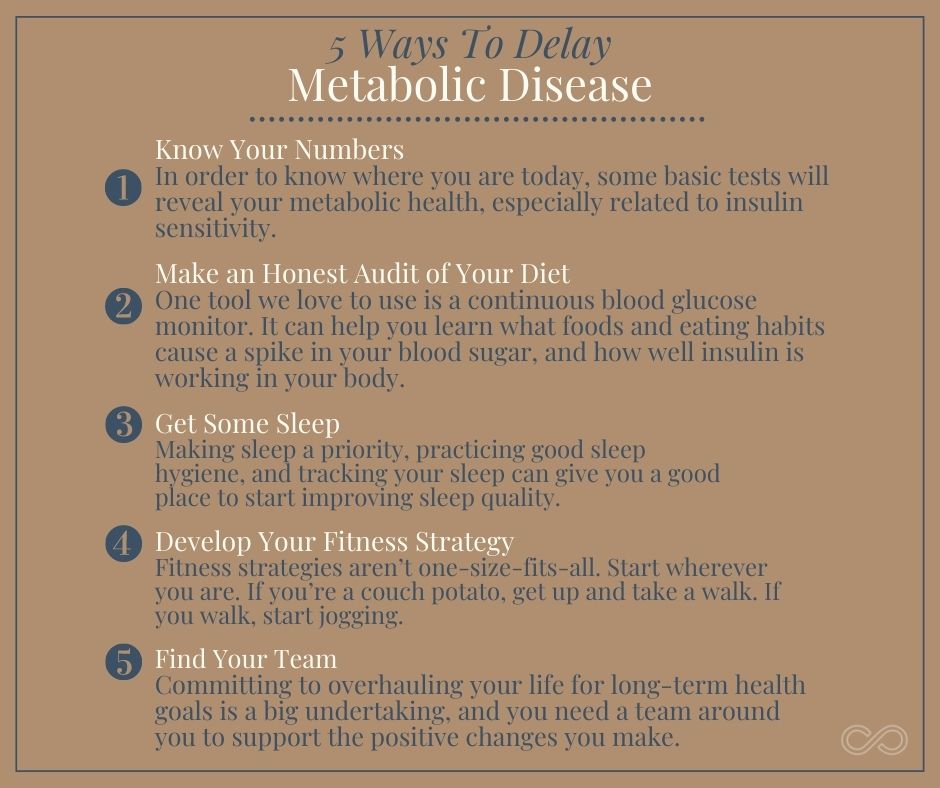
5 Ways To Delay Metabolic Disease
If you truly want to prevent metabolic disease, you’re never done delaying. Prevention only occurs if you’re successful at delaying long enough.
The number one, overarching way to delay metabolic disease is to actively, consciously increase your body’s response to the insulin it produces.
Below are five actionable steps you can take to improve insulin sensitivity and delay metabolic disease — maybe for good.
1. Know Your Numbers
In order to know where you are today, some basic tests will reveal your metabolic health, especially related to insulin sensitivity. These tests include:
- Fasting insulin levels.
- Fasting glucose levels.
- Fasting lipid panels.
- Inflammatory markers.
- Thyroid function.
- Sex hormones.
It’s also important to find a doctor who can accurately interpret this data for you.
2. Make an Honest Audit of Your Diet
Taking an honest look at your eating patterns can help you discover places to take action. Start by asking yourself questions like:
- Do I eat to sustain my life?
- Is my diet mapping me closer to my goals, or farther away?
- To what degree is diet affecting my insulin sensitivity?
- Am I eating high-quality food?
- What environments or habits do I need to change?
One tool we love to use is a continuous blood glucose monitor. It can help you learn what foods and eating habits cause a spike in your blood sugar, and how well insulin is working in your body.
Another strong recommendation we have for anyone going on the offense related to insulin sensitivity and metabolic disease is intermittent fasting. By restricting the hours in which you eat, you provide your body with those periods of scarcity we don’t naturally come by in today’s world. Your body has time to reset and begin working efficiently again.
3. Get Some Sleep
Sleep is so underrated, yet so important. One reason is sleep’s role in insulin sensitivity. Getting enough restorative, high-quality sleep optimizes your hormonal environment and helps reset that insulin sensitivity.
Making sleep a priority, practicing good sleep hygiene, and tracking your sleep can give you a good place to start improving sleep quality.
4. Develop Your Fitness Strategy
Fitness strategies aren’t one-size-fits-all. Start wherever you are. If you’re a couch potato, get up and take a walk. If you walk, start jogging.
Wherever you are, just take the next step. Be intentional about moving your body. Push a little further and challenge yourself to do a little more each day. Work to maximize your skeletal muscle, because skeletal muscle is the antidote to insulin.
5. Find Your Team
Simon Sinek famously said, “Failure we can do alone. Success always takes help.”
Everyone needs help. We’re social, tribal creatures, and we need support.
Committing to overhauling your life for long-term health goals is a big undertaking, and you need a team around you to support the positive changes you make.
Find your team — whether that’s a general practitioner, a trainer, a dietician, a therapist, or anyone else — to support you as you navigate the tests, dietary modifications, fitness strategy, and sleep improvement necessary for fighting metabolic disease.
The Takeaway: Develop a Strong Offense To Delay Metabolic Disease
Metabolic disease is insidious, and if you let up the pressure, it will take every opportunity to creep in.
Maintaining a strong offense isn’t easy, but it’s worth it. It’s the difference between living with metabolic disease for 5–10 years at the end of life, or for 30–40 years starting in middle age.

Dr. Aaron Wenzel is a concierge physician specializing in the care of fast-moving entrepreneurs, executives, and public figures in the Nashville, TN area. Dr. Wenzel’s diverse life experience and extensive training in family medicine, emergency care, nutrition, and hormone replacement therapies give him the unique platform to provide unmatched care for his patients.