You might think checking blood sugar is exclusively for those with diabetes. But a growing number of high-performing, “glucose-curious” individuals have begun monitoring this crucial metric not for disease management but for health optimization.
How? By taking advantage of the same tool diabetics use: a continuous glucose monitor (CGM).
CGMs provide data about what’s going on in your body in real time, allowing you to discover, track, and respond to your unique metabolic landscape. And because optimized blood sugar is the holy grail of health, this creates an unprecedented opportunity for you to directly and intelligently influence your overall health and longevity.
Blood Sugar and CGMs: How It All Works
CGMs are small, disc-like devices, usually one inch or less in diameter, that adhere to your skin for an established time period. Attached to each disc is a tiny filament, which inserts just under the skin to monitor your glucose levels. As the filament gathers information, the disc wirelessly transmits that data to a dedicated display device or smartphone app for you to read.
That’s CGMs. But let’s also do a quick review of blood sugar (glucose) to make sure we’re all on the same page.
When you eat sugar or other carbohydrates, your body breaks the food down and releases its glucose into your bloodstream. Your pancreas then sends out a hormone called insulin to help drive the glucose from your bloodstream into your cells to be made into energy.
This is the normal process, which involves a natural elevation of blood sugar after meals, followed by a return to baseline within an hour or two.
The trouble comes when your glucose levels stay chronically elevated over time. Your cells become less and less sensitive to insulin, eventually leading to insulin resistance and putting you on the path toward diabetes.
We start to worry when we see spikes above 160 or spikes that stay high for hours at a time. If your day looks something like breakfast → snack → lunch → snack → dinner → dessert, and you’re seeing spike after spike after spike, you’ll know you need a metabolic change. But a few reasonable spikes of around 140 to 160 after meals (and that drop back down within two hours) represent the healthy ebb and flow of your metabolism.
Why CGMs Matter Beyond Diabetes
The CGM use case for diabetics is pretty clear: monitor blood sugar so insulin or food can be taken at the right times to maintain safe and healthy levels. But what about for people who don’t have to take insulin?
If everyone reacted the exact same way to everything they ate, perhaps there wouldn’t be as much argument for CGM use outside of diabetes. But the truth is, calories in aren’t always calories out. Factors like genetics, baseline metabolic health, insulin resistance, and even gut health mean one person’s biology reacts differently to inputs than another’s.
Yes, we can probably all expect dessert to raise our blood glucose, but how much? And what about sweet potatoes? French fries? One person may eat a few fries and see their blood sugar skyrocket. Another may devour a large amount yet maintain at a relatively normal level.
As such, even metabolically pristine individuals can learn a lot from a CGM, not to mention those struggling with insulin resistance or stubborn excess weight. The data offers a peek inside the trends and fluctuations of your blood sugar as influenced by your daily habits, providing you the insights needed to avoid and potentially reverse flagging metabolic health.
This is also where precision medicine comes into play. The more data I, as your physician, have about you, the better we can work together to tailor a fitness and nutrition plan that suits your unique biology and goals.
CGM Aha Moments: My Personal Experience
As I’ve used and assessed various CGM devices, I’ve made some eye-opening personal discoveries along the way. Here are just a few:
Protein Forward Matters
One night, I was cooking a big family meal with steaks. I pulled the steaks out of the oven to rest, but while waiting, I cut into them and had a few bites. Then we sat down to a huge meal with some carb-heavy foods.
When I checked my CGM, my blood glucose had barely spiked from all those carbs. Shocked, I realized it was the impact of consuming those few bites of protein 10 to 15 minutes before the carbs, which many studies confirm.
Brown Rice vs. White Rice
Another personal discovery was that white rice caused a much stronger glucose response in me than brown rice with the same carb load. This is likely because brown rice contains the germ and bran of the rice, giving it more fiber, a bit of protein, and a bit more fat and micronutrients. Individual responses matter, but personally, I spike far worse with white rice than brown rice.
The Dessert Experiment
My wife and I once went to Cold Stone Creamery after dinner, both wearing CGMs. Many of our glucose spikes had been pretty similar, as we ate the same meals.
For dessert, though, she got a cookies-and-cream milkshake. I got a raspberry sorbet.
To my surprise, my glucose spiked worse than at any other time in that two-week monitoring period. But my wife’s spike wasn’t too bad.
Thinking it through, I realized the milkshake, despite being indulgent, had fat and protein to both moderate the glucose spike and bring it back to baseline more quickly. The sorbet was just a huge sugar load hitting my bloodstream all at once.
That was my last raspberry sorbet of the season.
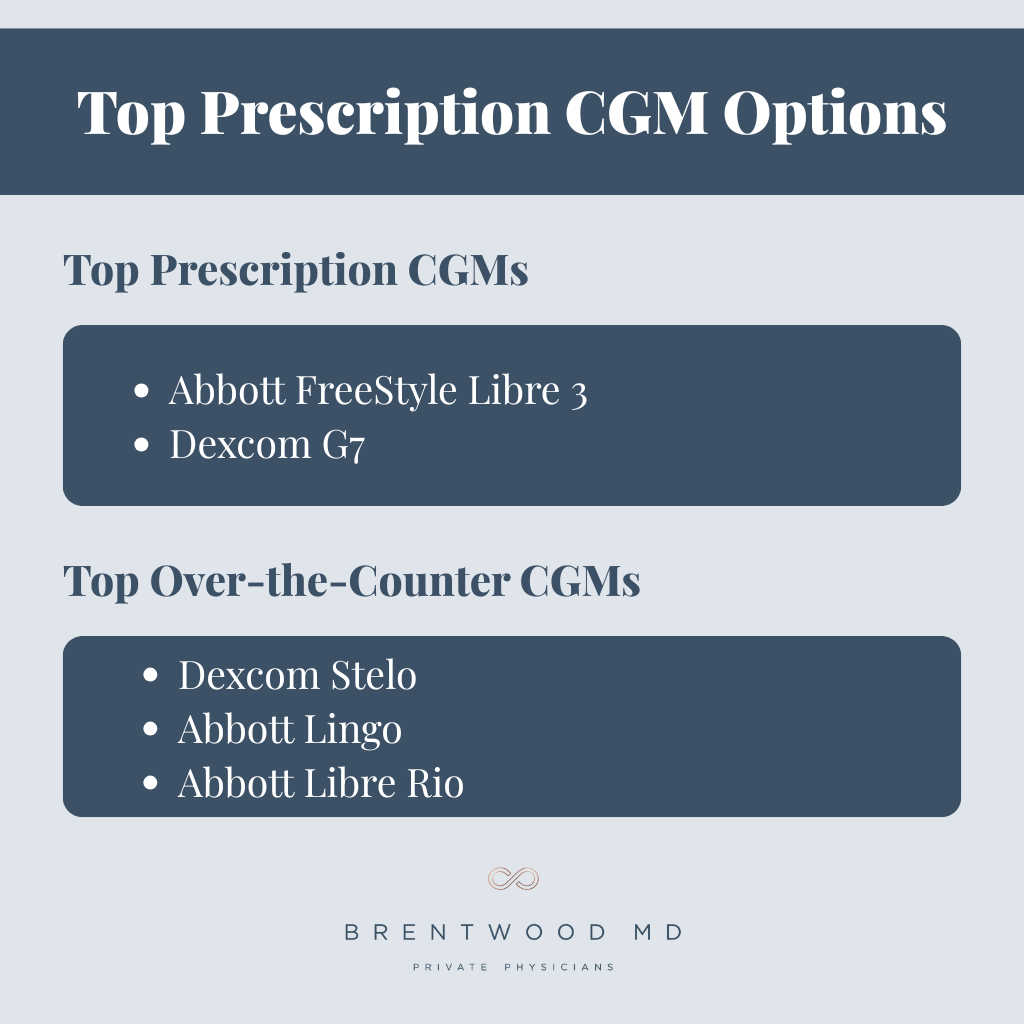
Top Prescription CGM Options
Two prescription CGMs currently dominate the market. These are designed for managing both type 1 and type 2 diabetes, and they’re typically covered by insurance for diabetics on insulin.
Both models include alarms for low blood sugar, which is critical for insulin-dependent patients, but they work just fine as monitors for those without diabetes as well. Here are some quick stats on each:
Abbott FreeStyle Libre 3
- Wear Time: 14 days
- Reading Frequency: Every 1 minute
- Current Cash Cost: Varies; around $155 for a 28-day supply
The FreeStyle Libre 3 also doesn’t have as robust a set of sharing features and isn’t as well-integrated with insulin pumps as its competitor, the Dexcom G7. Also, when the Libre 3 stops, it stops. There’s no grace period when the sensor’s time ends.
Dexcom G7
- Wear Time: 10 days
- Reading Frequency: Every 5 minutes
- Current Cash Cost: Varies; around $180 for a 30-day supply with manufacturer coupon
The Dexcom G7 is a great tool with excellent insulin pump integration and well-developed sharing features for caregivers and family. It also has a 12-hour lead time for transitioning off, so no data points go missing between sensors.
Top Over-the-Counter CGM Options
Here’s where it gets very cool for the glucose-curious among us who don’t have diabetes or aren’t on insulin. You actually don’t have to see a doctor to get data on your glucose levels anymore.
Over-the-counter CGMs are designed for users who simply want to monitor their blood sugar but don’t take insulin for diabetes. As such, they all omit the low-glucose alarm, and they generally aren’t covered by insurance.
Dexcom Stelo
- Wear Time: 15 days
- Reading Frequency: Every 5 minutes (updates sent every 15 minutes)
- Current Cash Cost: $99 for a one-month supply
- Glucose Range: 70 to 250 mg/dL
Though it updates less often than other models, the Dexcom Stelo still provides plenty of actionable data for your health. Its smartphone app offers helpful features like spike detection, Oura Ring partnership, and a Smart Food Log. If you experience glucose levels outside the app’s range, you can visit Dexcom’s Clarity platform.
Abbott Lingo
- Wear Time: 14 days
- Reading Frequency: Every 1 minute
- Current Cash Cost: $89 for a one-month supply
- Glucose Range: 55 to 200 mg/dL
The Abbott Lingo also comes with a useful app, which offers weekly insights, Apple Health syncing, and a diet and exercise log. However, you won’t be able to view glucose spikes above 200 mg/dL.
Abbott Libre Rio
- Wear Time: 15 days
- Reading Frequency: Every 1 minute
- Current Cash Cost: Unclear; possibly similar to the Lingo
- Glucose Range: 40 to 400 mg/dL
The downside of the Libre Rio is that, though it received FDA approval in 2024, Abbott hasn’t released it as of the end of 2025. When they do, however, the Libre Rio will have the widest glucose reading range on the OTC market, making it a valuable and comprehensive option.
What to Do With the Data: Actionable Strategies
Having the data is one thing. Knowing what to do with it is another. If you decide to use a CGM to improve your metabolic health, here are some tips for taking action:
When You See a Big Spike
First, evaluate the stimulus. What did you eat? Try the same meal again, but cut the carbs in half or add protein before the meal. Did that change anything? Embrace the experiment.
Other ways to blunt spikes:
- Save carbs for the last part of your meal.
- Move after a meal.
- If you notice prolonged nighttime spikes, eat earlier in the evening.
- Reserve carb-heavy meals for days when you can move afterward.
The goal is meals that produce a gentle rise and gradual return to baseline, rather than a succession of major spikes and drops.
Watch Out for Stress
Perhaps surprisingly, stress can have a major impact on glucose levels.
My Brentwood MD colleague, Dr. Wright, shared that his CGM once noted a glucose spike after his son realized he’d forgotten something he needed for school… while on the way there. They returned home and everyone got to their destinations successfully, but Dr. Wright was surprised by how much even that mild stressor affected his glucose. How much more, then, must chronic stress impact blood sugar and insulin sensitivity over time!
When you notice situations like these, remember that mindful strategies can help. Even 10 minutes of walking or breathing exercises can reduce stress and help flatten that rise.
Sleep and Shift Work
Night shift workers and people who struggle with sleep loss often have elevated fasting glucose levels, are more insulin resistant at baseline, and experience larger spikes after meals.
If you’re a night shift worker:
- Expect higher spikes from overnight meals.
- Prioritize protein and fat over carbs during those meals.
- Aim for one to two nights per week with normal sleep and no late eating.
These habits can help stabilize your blood glucose and insulin needs and help prevent progression of worsening blood sugar control over time.
When You See a Big Drop
When you see crashes or sharp drops, the most common causes are:
- Intense exercise in a fasted or low-glucose state
- High carb load with little protein or fat, creating a spike and reactive drop afterward
The goal is to aim for meals that produce a gentle rise and a gradual return to baseline. Having carbs, fat, and protein in a meal (even if you’re intentionally carb-loading) will help achieve that.
Patterns Over Perfection
You won’t be able to chase down every glucose spike and eliminate it. And you don’t need to. For metabolically healthy adults, a rare, brief spike after a celebration meal is a data point. It’s not a failure.
Yes, consistent or long-lasting spikes merit attention, but you don’t need to be discouraged by every elevation. Remember, fluctuation is normal. Focus on overall patterns rather than perfection.
Friction Points: When CGMs Might Not Be the Right Fit
Despite their benefits, a few friction points mean CGMs may not be right for every person:
- Alarm fatigue: The low-glucose alarms in prescription CGMs can unnecessarily interrupt sleep for non-insulin-taking individuals, which is one reason the OTC options may be preferable for the glucose-curious.
- Stress and anxiety: Some people find that continuously monitoring their blood glucose causes excess stress and anxiety, which is counterproductive for optimizing blood sugar.
- Risk of restrictive eating: For some, CGMs could lead to over-restricting food intake to reduce spikes. Remember, you still have to eat food, and it’s important to see those ebbs and flows of your blood glucose.
Getting Started With a CGM
You really can’t manage what you don’t measure.
CGMs allow you to connect your blood glucose levels to your daily lifestyle choices in a measurable, visible way. The insights from these devices allow you to take more proactive control of your metabolic health, especially when you work with a healthcare team who provides useful support and advice during the process.
If you’re one of our members at Brentwood MD and interested in a CGM, we can provide you a Libre 3 and Dexcom G7 sample to try for free. For others interested in a CGM for health optimization, all the OTC products mentioned above are excellent options, but the Libre Rio will likely be my favorite device once it comes on the market.
Whether you’re trying to prevent diabetes, optimize athletic performance, or just understand your body better, CGMs offer a window into your metabolic health that wasn’t accessible to most people just a few years ago. The data is powerful. What you do with it is even more powerful.

Dr. William Pierce is a board-certified Family Medicine physician with experience in Emergency Medicine who joined Brentwood MD in 2025. He specializes in providing comprehensive, personalized care that combines preventive health strategies with acute medical expertise. Dr. Pierce is committed to building enduring patient relationships grounded in trust, clinical excellence, and collaborative health management.