Download file | Play in new window | |
We spend a lot of time talking about top killers like cancer, heart disease, and dementia on this blog. But what about osteoporosis?
Many people are aware that bone density loss poses an increasing risk as you age. But can osteoporosis kill you?
While you won’t find it on any official “top killers” list, that’s only because people aren’t talking about osteoporosis this way — yet.
The loss of bone density joins the more notorious deadly diseases as a leading cause of death among the aging population, especially for women. In fact, about half of women over age 50 will develop osteoporosis, making it a severe and significant threat to longevity.
If you want a vibrant and fulfilling second half of life, bone health is essential. Fortunately, you can start taking steps right now to reduce your osteoporosis risk.
 What Osteoporosis Is and When It Starts
What Osteoporosis Is and When It Starts
We’re musculoskeletal creatures, with all our elements built on a foundation of bone, muscle, tendon, and ligament. Without a strong foundation, we can’t expect to function optimally.
It’s much like a house: All the window dressing and throw pillows and advanced electrical wiring in the world won’t matter if the infrastructure is falling down around it.
Adults reach their peak bone mass by around age 35. After that, it starts a natural process of decline — but that doesn’t make osteoporosis inevitable. And it doesn’t happen overnight.
DOWNLOAD OUR FREE EBOOK
Concierge Medicine is the future of healthcare.
Learn more about this refreshing alternative to traditional primary care, and decide if it's right for you.
Key Considerations to decide...
Is Concierge Medicine Right for You?
Bone loss happens gradually, usually starting around age 40. As we age, our rate of bone loss increases while our rate of bone formation decreases. By age 50, bone loss outpaces bone formation. This is the time when many women develop the precursor to osteoporosis: osteopenia.
With osteopenia, bones become thinner and bone mineral density falls below normal. However, the condition is considered reversible.
If you continue to lose bone tissue, however, osteoporosis eventually develops, leaving you with brittle, fragile bones that are highly susceptible to fracture.
For a more detailed picture, imagine looking at a healthy bone under a microscope. Instead of a solid wall of white, you’d see a honeycomb pattern. This is the natural structure of bones at a microscopic level.
With bone loss, the spaces in that honeycomb matrix become wider and wider, making the bones more and more porous. Hence the name osteoporosis: “osteo” for “bone” and “porosis” because of that increasing porousness.

How Can Osteoporosis Kill You?
Weak, fragile bones increase your risk of fracture. The biggest danger of osteoporosis is the risk of something like a normal fall causing a fracture, especially a hip fracture.
Hip fractures significantly increase an older person’s risk of dying, most notably within the first three months to a year after the incident. This can be due to pneumonia, blood clots, failed surgery, or even sepsis from a bed sore. Plus, once you break a bone in your pelvic floor, you’re not moving. This puts you on the fast track to a reduced life expectancy.
Studies suggest that about 1 in 3 women and 1 in 5 men age 50 and older will break a bone due to osteoporosis.
How Is Osteoporosis Diagnosed?
Many women only discover they have osteoporosis when they break a bone. Some don’t discover it even then (osteoporosis is woefully underdiagnosed in much of the world).
The best strategy to detect (and prevent!) osteoporosis is a proactive one. Doctors can measure your bone density and strength through a noninvasive test called a DEXA scan, which compares X-rays of the bones in your lumbar spine, hips, and wrists to those of a young, healthy adult of the same sex.
Though DEXA scans are currently recommended for women over 65, you can opt to have one before you reach menopause. This provides you and your doctor with some runway to address any early warning signs and a baseline for comparison against later scans.
 Risk Factors for Osteoporosis
Risk Factors for Osteoporosis
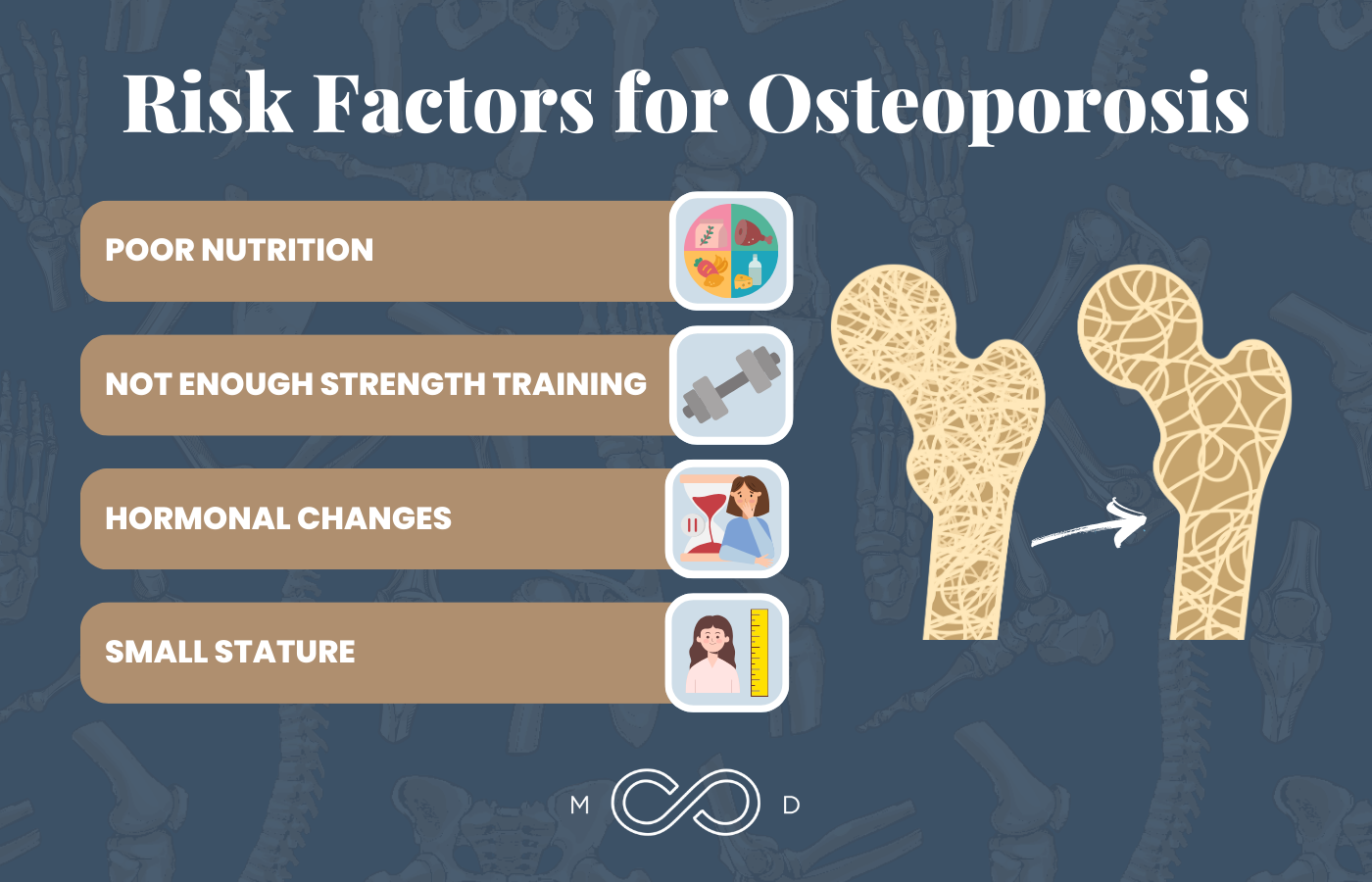
Osteoporosis doesn’t affect everyone equally, so it’s important to know your risk factors, adjust what you can, and compensate for what you can’t. The following are some of the top risk factors for osteoporosis, and most are within your power to address.
Risk Factor #1: Poor Nutrition
Calcium is the primary mineral in bone and an essential nutrient in your diet. If you’re not consuming enough, your body will steal calcium from your bones. Women who avoid dairy products or who don’t eat enough leafy greens may not get enough calcium.
Vitamin D3, which is actually a hormone, is necessary for the absorption of calcium. We get some from our diet, and our bodies manufacture it when our skin is exposed to sunlight. In our very indoor culture, however, I rarely encounter individuals with normal or optimal vitamin D levels unless they take a supplement.
Besides poor diet, mineral depletion in our soil reduces the availability of these vital micronutrients in our foods, contributing to deficiencies that affect bone health.
Risk Factor #2: Not Enough Strength Training
Strength training and weight-bearing exercises are crucial both for laying down new bone and for preserving what you have.
Weight-bearing exercise is any activity in which your feet touch the ground, so swimming and biking won’t do the trick here. However, low-impact activities like walking and light gardening work well, along with higher-impact activities such as dancing and running.
Strength training involves challenging your muscles with weights and activities that involve resistance, like squats. Women sometimes gravitate toward cardio and avoid strength training, worrying it will make them bulky. It won’t. Our very own Jen has been strength training for a year and a half and can attest to this. What you will get is more muscle tone and definition — and stronger bones.
Risk Factor #3: Hormonal Changes
One of the major contributors to postmenopausal osteoporosis is the hormonally barren environment women find themselves in. Everything that keeps you young, healthy, and vibrant — mainly estrogen, progesterone, and testosterone — begins to decline.
These hormones are involved in bone building. As your levels decline, you lose the hormonal components of bone health and equilibrium. This is one of the main reasons women typically outpace men in bone loss in the back half of life.
One surprise to many is that while estrogen is important for bone health, testosterone plays an even bigger role — laying down 50% more bone than estrogen! So, a discussion about optimal hormone levels for women’s bone health may even include testosterone.
Finally, an off-kilter thyroid can affect calcium metabolism and regulation, which of course affects bone health. It doesn’t help that thyroid health is poorly understood in conventional medicine, which often overlooks subclinical hypothyroidism.
Risk Factor #4: Small Stature
Women with small frames have an enhanced risk of osteoporosis. When you’re small, trim, and metabolically pristine, you have a lower risk for cardiovascular disease, stroke, and many other life-limiting conditions. Unfortunately, you have a higher risk of losing bone density.
So while you may not have a heart attack, you’re at real risk from something as simple as tripping over a curb.
This is one area in which larger women have an advantage. Bones adapt to the amount of pressure they’re forced to bear (hence the benefit of strength training), so heavier women develop thicker and heavier bone density. They tend not to develop osteoporosis or suffer hip fractures.
 Tips for Reducing Your Osteoporosis Risk
Tips for Reducing Your Osteoporosis Risk
Put It on Your Radar
Awareness is the first step in any health journey. When it comes to your bones, the first goal is to prevent osteopenia. Have a conversation with your doctor about your risk and where you are on the spectrum of normal, optimal bone health. Osteoporosis is rooted largely in modifiable factors, so proactive awareness really does make a difference.
Fix Your Nutrition
Women who avoid dairy products, don’t consume enough fish or leafy greens, or don’t see enough sunlight likely aren’t getting the calcium and vitamin D necessary for healthy bones. So get your levels checked and supplement if necessary. We recommend 5000 IU of vitamin D3 daily.
Pro tip: Since we’re big proponents of intermittent fasting, it’s important to note that you must take vitamin D while you’re consuming calories. Specifically, fat facilitates D3 absorption, so take this supplement alongside a fatty meal.
Heed Your Hormone Levels
Postmenopausal hormone depletion is a tremendous, overlooked disadvantage for women’s bone health. But in many cases, you and your doctor can manage it through a thoughtful discussion and approach regarding hormone optimization.
Hormone replacement therapy (HRT) isn’t without controversy, but we’ve done hundreds of hours of deep-dive research, and we believe it makes sense in most cases. I recommend finding a doctor who can help you safely optimize your hormones. Get yourself in front of someone who’s willing to at least have the conversation so you can properly assess your unique risks and potential benefits.
Additionally, you should know your thyroid levels. Discuss with your doctor whether your thyroid is operating optimally for calcium metabolism and regulation.
Start Strength Training
Feeling powerful physically isn’t just a man thing. It’s a human thing, and women should absolutely enjoy the immense benefits of lifting weights.
Strength training is a beautiful process of pursuing the strength our bodies require and getting confirmatory feedback. Not only are we doing right by our musculoskeletal system, but we’re also uplifting our tone, attitude, and outlook on life.
Strength training can even help with the seemingly non-modifiable risk factor of stature. By loading their spines with additional pounds in exercises like squats, lunges, and deadlifts, women — especially smaller women — challenge their bones and increase their bone strength more than their body weight alone would accomplish.
Our bodies don’t like to waste energy, so they don’t make bones that are stronger than we need. A 120-pound frame simply isn’t enough weight to force your bones to get stronger and resist the depletion of age, but added pounds send them signals that they have to do more.
If you’re looking to get started with strength training, there are amazing trainers who would love to guide you in a way that’s safe and aligned with your personality and goals. You’ll likely unlock some physicality you forgot you had!
Jen’s Journey to Justice for Her Bones
Our very own Jen Justus is a great example of a woman who looked at her fear related to strength training and stepped right into it — and then kept showing up. It became less scary over time, and suddenly, being strong became part of who she is. She’s found it’s a great confidence booster, especially as a female.
Working with a trainer may not come cheap, but it’s something Jen prioritized in the name of health.
Your health is very much an “invest now or pay later” proposition. Investing in bone health now will pay dividends in how you look, feel, and function during the second half of life.
Can Osteoporosis Kill You? Yes, but You Can Fight It
I hope you found some inspiration to tackle your bone health, starting now. Though less of a specter than other leading killers — like cancer — osteoporosis poses a real threat to health and longevity.
So, yes, osteoporosis can kill you — but you can take action today to stop it. While some non-modifiable factors, like genetics, do play a role, the health of your bones rests largely in your hands.
Make a plan and work with your physician to keep your foundation solid and strong for as long as possible. Your future self will thank you.

Dr. Aaron Wenzel is a concierge physician specializing in the care of fast-moving entrepreneurs, executives, and public figures in the Nashville, TN area. Dr. Wenzel’s diverse life experience and extensive training in family medicine, emergency care, nutrition, and hormone replacement therapies give him the unique platform to provide unmatched care for his patients.